NSR:乙肝病毒相关性肝细胞癌的肿瘤微环境
2014-10-07 王小凡 《国家科学评论》
HBV调节肿瘤微环境中细胞组分的活性 肝细胞癌(hepatocellular carcinoma,HCC)是世界上第五大常见恶性肿瘤,为癌症死亡第三大原因。 与很多癌症不同, 肝细胞癌的发生与慢性肝脏疾病进程密切相关。乙型肝炎病毒(hepatitis B virus,HBV)感染是HCC最重要的病因之一,HBV诱发肝癌通常伴随或继发于长期的慢性肝炎(chronic he
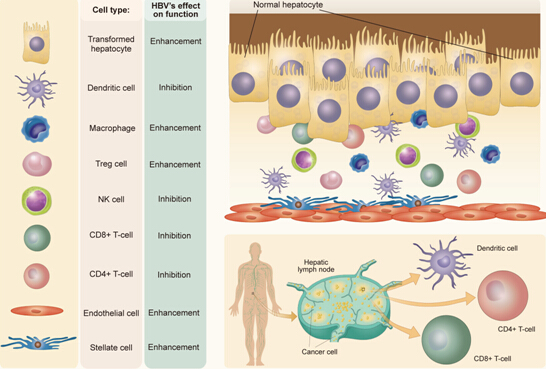
HBV调节肿瘤微环境中细胞组分的活性
肝细胞癌(hepatocellular carcinoma,HCC)是世界上第五大常见恶性肿瘤,为癌症死亡第三大原因。 与很多癌症不同, 肝细胞癌的发生与慢性肝脏疾病进程密切相关。乙型肝炎病毒(hepatitis B virus,HBV)感染是HCC最重要的病因之一,HBV诱发肝癌通常伴随或继发于长期的慢性肝炎(chronic hepatitis)、炎症反应(inflammation)和肝硬化(cirrhosis)。近年的研究表明,除了直接影响肝细胞癌变之外,HBV感染 还通过调控肿瘤微环境来影响肝细胞癌的发生,发展和转移。
美国杜克大学医学院王小凡教授在《国家科学评论》最新发表综述文章“乙型肝炎病毒相关性肝细胞癌的肿瘤微环境”(http://nsr.oxfordjournals.org/content/1/3/396.full),详尽阐述了近年来发现的HBV感染相关肝细胞癌肿瘤微环境中的细胞组分、非细胞组分及其相关作用机制。
该文中提到,HBV感染相关肝细胞癌肿瘤微环境中的细胞成分包括肿瘤浸润性淋巴细胞(Tumor-infiltrating lymphocytes)、树突状细胞(Dendritic cells,DCs)、巨噬细胞和库夫氏细胞Macrophages and Kupffer cells)、自然杀伤细胞(Natural Killer cells,NK cells)、肿瘤相关成纤维细胞(Carcinoma-associated fibroblasts ,CAFs)和肝脏星状细胞(Hepatic stellate cells,HSCs)及内皮细胞(Endothelial cells)等;非细胞组分主要有细胞因子(Cytokines)和趋化因子(Chemokines),生长因子(Growth factors)和其他可溶性蛋白(soluble proteins),微小RNA(microRNAs)及物理免疫微环境等。
王小凡教授指出,肝细胞癌形成背景复杂,肿瘤微环境还会随着肝细胞癌的发生、发展及转移等过程呈现出高度的动态变化和更为复杂的交互作用系统。HBV感染对于肝细胞癌微环境中细胞组分及非细胞组分的调控起着关键作用,可显著影响肝细胞癌的发展和预后。阐明这一交互系统中的主要成分及作用机制,分析动态变化的肿瘤微环境的共性及不同之处,对于发展更加有效、针对性更强的治疗方法意义重大。本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝细胞#
28
#相关性#
25
#细胞癌#
28
对啊,说的好简单
127
好象也没讲清楚吧
93