JAHA:颈动脉斑块和C反应蛋白在缺血性卒中和心肌梗死中的联合作用!
2018-05-18 xing.T MedSci原创
由此可见,同时存在亚临床动脉粥样硬化和CRP升高与IS和MI风险增加有关。将亚临床动脉粥样硬化和炎症生物标志物进行联合评估可改善心血管疾病的风险分层。
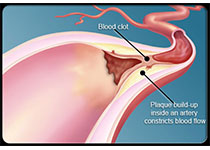
动脉粥样硬化和C反应蛋白(CRP)对缺血性卒中(IS)和心肌梗死(MI)风险的联合作用已被广泛研究。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是探讨CRP是否介导颈动脉斑块患者的事件风险,评估协同作用,并明确将CRP和颈动脉斑块加入后风险预测能力是否优于传统的危险因素。
研究人员测量了来自于Tromsø研究的1994年至2008年期间的10109例参与者的CRP和颈总斑块面积(TPA)。IS(n=671)和MI(n=1079)登记截止至2013年12月31日。在随时间变化协变量的Cox比例风险模型中,根据CRP(<1、 1-3和>3mg/L)和斑块状态(无斑块、中位数以下和以上的TPA),研究人员计算了MI和IS的风险比(HRS)。
多变量调整后的CRP>3与<1mg/L比较与IS(HR为1.84;95%可信区间为1.49-2.26)和MI(HR为1.46,95%可信区间为1.23-1.73)风险相关。中位数以上的TPA与无斑块比较与IS(HR为1.65;95%可信区间为1.36-2.01)和MI(HR为1.64,95%可信区间为1.41-1.92)风险相关。在存在斑块的参与者中,CRP调整最小程度的减弱了风险估计。CRP>3mg/L和TPA高于中位数的参与者MI和IS的发生率最高。TPA和CRP联合后的风险预测能力优于传统危险因素。
由此可见,同时存在亚临床动脉粥样硬化和CRP升高与IS和MI风险增加有关。将亚临床动脉粥样硬化和炎症生物标志物进行联合评估可改善心血管疾病的风险分层。
原始出处:
Agnethe Eltoft,et al.Joint Effect of Carotid Plaque and C‐Reactive Protein on First‐Ever Ischemic Stroke and Myocardial Infarction? JAHA.2018. https://doi.org/10.1161/JAHA.118.008951
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#缺血性卒#
40
#联合作用#
39
#缺血性#
35
#颈动脉#
49
学习一下谢谢
65
#AHA#
34
#颈动脉斑块#
40
#C反应蛋白#
37
#斑块#
41
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
53