精品指南:2017 GOLD慢性阻塞性肺疾病全球倡议解读,全新专家解读视频免费送!
2017-03-16 MedSci MedSci原创
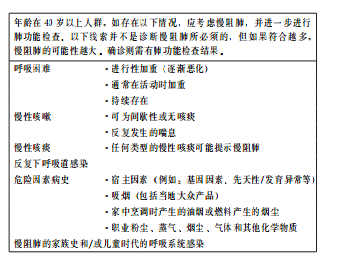
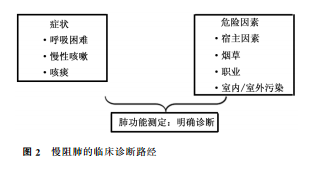
慢性阻塞性肺疾病全球倡议组织最新发布了2017版GOLD慢阻肺诊断治疗和预防的全球策略报告,文章包括对已经发布的2015版和2016版的更新。更新主要包括6部分内容。 【指南全文】 2017 GOLD慢性阻塞性肺疾病全球倡议:COPD诊断、治疗与预防全球策略 【指南解读】 自从2001年慢性阻塞性肺疾病全球倡议(GOLD)颁布第1版慢性阻塞性肺疾病诊断、处理和预防全球策
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#阻塞#
32
#专家解读#
29
慢阻肺的病因与宿主因素和环境暴露之间的关系。
73
#GOLD#
34
好好学习,涨知识
59
新版COPD指南变化还是比较多。
70
很好的学习资料,谢谢了。
63
学习了,非常好的研究,谢谢分享
76
谢谢分享,学习了
29
谢谢分享
26