Blood:Wilms'' tumor1基因突变或剂量不足时需额外的基因突变协同诱导白血病发生
2018-08-02 MedSci MedSci原创
中心点:Wt1杂合子会丧失年龄依赖性的干细胞自我更新增强的特性。Wt1-半剂量效应不足白血病需要额外的事件来促进造血转化。摘要:遗传研究已发现在急性髓系白血病(AML)患者中会反复发生体细胞突变,包括WT1(Wilms肿瘤1)基因。WT1突变导致白血病发生的分子机制尚未完全阐明。Elodie Pronier等人对Wt1基因剂量在稳定造血和病理性造血中的作用进行研究。Wt1杂合子会丧失年龄依赖性的干
Wt1杂合子会丧失年龄依赖性的干细胞自我更新增强的特性。
Wt1-半剂量效应不足白血病需要额外的事件来促进造血转化。
摘要:
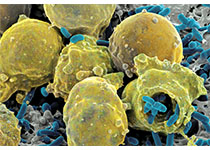
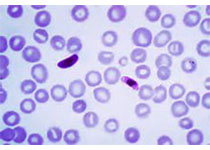
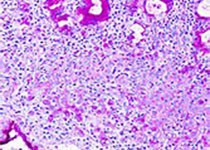
遗传研究已发现在急性髓系白血病(AML)患者中会反复发生体细胞突变,包括WT1(Wilms肿瘤1)基因。WT1突变导致白血病发生的分子机制尚未完全阐明。Elodie Pronier等人对Wt1基因剂量在稳定造血和病理性造血中的作用进行研究。
总而言之,本研究为Wt1缺失型白血病的发生机制提供新的见解,并阐述了诱导Wt1半剂量效应不足干/祖细胞转化所需要的额外事件。
原始出处:
Elodie Pronier,et al.Genetic and epigenetic evolution as a contributor to WT1-mutant leukemogenesis.Blood 2018 :blood-2018-03-837468; doi: https://doi.org/10.1182/blood-2018-03-837468
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#白血病发生#
29
#Tumor#
38
认真学习,不断进步,把经验分享给同好。点赞了!
79
学习
68
阅
82