Nat Nanotechnol:研发纳米喷胶,有望抑制术后肿瘤复发
2018-12-11 佚名 学术经纬
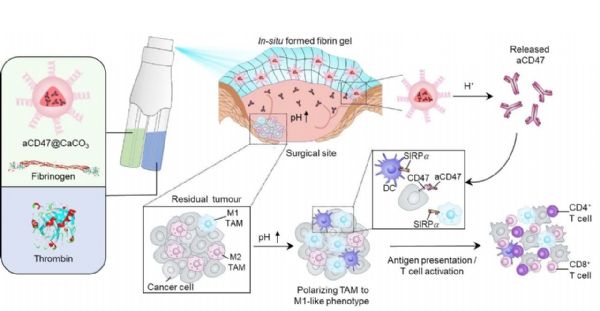
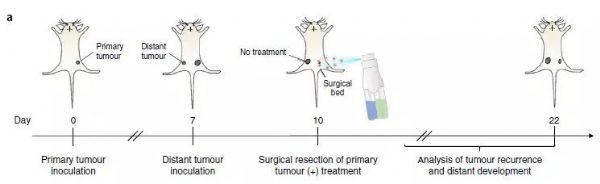
今日,《自然》子刊《自然·纳米技术》(Nature Nanotechnology)在线刊登了一项创新抗癌研究:加州大学洛杉矶分校(UCLA)华人学者顾臻教授与其团队开发出了一种新型癌症免疫治疗策略。通过在肿瘤切除部位喷洒喷雾,快速形成凝胶,并通过包埋其中的纳米颗粒缓释抗体药物,研究人员在动物模型上验证了该种喷剂能靶向手术后的残余癌细胞,显着抑制癌症复发和潜在的转移。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
33
#TEC#
39
#肿瘤复发#
51
#研发#
33
学习了谢谢
55