EuroIntervention:TARGET I研究显示FIREHAWK®支架不劣于依维莫司洗脱支架
2014-01-06 箫砚 dxy
9个月随访之后晚期官腔丢失比较(FIREHAWK®支架与XIENCE V®支架) 研究要点: 1、FIREHAWK®支架是新型生物可降解涂层靶向释放雷帕霉素的新型支架。FIREHAWK®支架采用钴络合金材料、表面刻槽载药和可降解聚合物的独特设计。药物的(雷帕霉素)靶向释放仅针对血管壁方向进行释放,大大降低了药物剂量。 2、TARGET I 研究旨在评估FIREHA
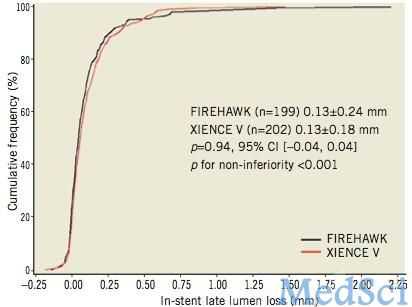
9个月随访之后晚期官腔丢失比较(FIREHAWK®支架与XIENCE V®支架)
研究要点:
1、FIREHAWK®支架是新型生物可降解涂层靶向释放雷帕霉素的新型支架。FIREHAWK®支架采用钴络合金材料、表面刻槽载药和可降解聚合物的独特设计。药物的(雷帕霉素)靶向释放仅针对血管壁方向进行释放,大大降低了药物剂量。
2、TARGET I 研究旨在评估FIREHAWK®支架与XIENCE V®支架(EES)对单发冠脉病变(病变既往未接受治疗)患者的疗效。
3、本项研究结论为,从9个月后晚期官腔丢失发生率考虑,SES FIREHAWK支架不劣于EES XIENCE支架。
FIREHAWK®支架是一种生物可降解涂层靶向释放雷帕霉素的新型支架(SES)。FIREHAWK®支架采用钴络合金材料、表面刻槽载药和可降解聚合物的独特设计。药物的(雷帕霉素)靶向释放也仅针对血管壁方向进行释放,大大降低了药物剂量。TARGET I 研究旨在评估FIREHAWK®支架与XIENCE V®支架(EES)对单发冠脉病变(病变既往未接受治疗)患者的疗效。【原文下载】
TARGET I研究共纳入458名患者,这些患者均存在单支冠脉损伤、病变冠脉既往未曾接受血管成形或支架植入。患者冠脉岁上的长度<=24mm,宽度>=2.25)。主要研究终点是随访研究9个月之后晚期官腔丢失(LLL)。次要终点是目标冠脉治疗失败,治疗失败的定义事件包括心源性死亡、靶血管心梗(TVMI)或缺血驱动的血管重建(iTLR)等组成的复合事件。患者被随机分成两组,一组接受FIREHAWK®支架治疗,一组接受XIENCE V®支架治疗。
研究结果显示,9个月后晚期官腔丢失发生率,FIREHAWK®支架小于XIENCE V®支架;随访12个月之后,两组之间心源性死亡、靶血管心梗(TVMI)或缺血驱动的血管重建(iTLR)等组成的复合事件发生率相似。随访期间,两组均为发现确定或可能存在的支架血栓。
本项研究结论为,从9个月后支架内再阻塞发生率考虑,SES FIREHAWK支架不劣于EES XIENCE支架。12个月随访结果显示,两组之间的临床终点发生率均比较低。
研究背景:
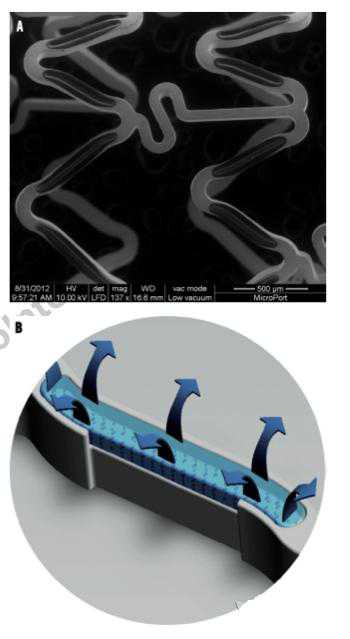
图A,FIREHAWK支架的细节展示
A)显微图片:FIREHAWK®支架不同连杆之间采用S型设计,该设计有助于使支架更加灵活,可减少支架正弦曲线之间的距离,增加支架与病变部位的接触面积。(扫描电子显微镜下,original magnification ×150)
B)FIREHAWK®支架采用单面刻槽涂层设计。刻槽发挥的作用包括:1,载药 2,靶向释放进针对血管壁方向药物的作用。
药物洗脱支架(DES)与金属裸支架相比,其通过释放抗增生药物已经显著减少冠脉再狭窄事件的发生,此外,心梗以及死亡等不良事件发生率也降低。但是,第一代药物洗脱支架与持续性炎症反应、内皮修复延迟存在相关性,这可能导致后迟发晚期以及极晚期支架血栓发生。
随着支架开发技术以及无创造影技术的提高,以及生物可降解材料的引用,新型药物支架与第一代药物洗脱支架相比,已经有了很大提高。
FIREHAWK®支架(MicroPort Medical, Shanghai, China) 是上海微创公司最新研发的生物可降解涂层靶向释放雷帕霉素的新型支架。FIREHAWK®支架采用钴络合金材料、表面刻槽载药和可降解聚合物的独特设计。药物的(雷帕霉素)靶向释放仅针对血管壁方向进行释放,大大降低了药物剂量。
TARGET I 研究旨在评估FIREHAWK®支架与XIENCE V®支架(Abbott Vascular, Santa Clara, CA, USA) 对于既往未接受过血管成形或支架植入术的单发冠脉病变患者的疗效。
原文出处:
Gao RL, Xu B, Lansky AJ, Yang YJ, Ma CS, Han YL, Chen SL, Li H, Zhang RY, Fu GS, Yuan ZY, Jiang H, Huo Y, Li W, Zhang YJ, Leon MB; TARGET I Investigators.A randomised comparison of a novel abluminal groove-filled biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: clinical and angiographic follow-up of the TARGET I trial.EuroIntervention. 2013 May 20;9(1):75-83. doi: 10.4244/EIJV9I1A12.【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#依维莫司洗脱支架#
24
#target#
29
#洗脱支架#
40
#EHA#
21