发热、皮疹伴快速进展型间质性肺炎,小心这类疾病!
2019-01-23 韩茜 毛萌萌 南山呼吸
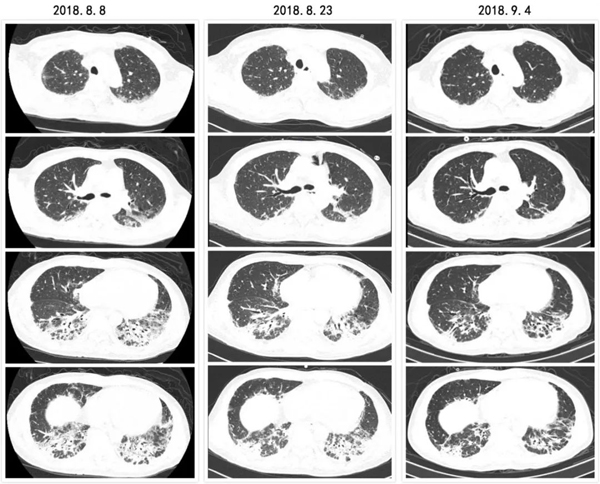
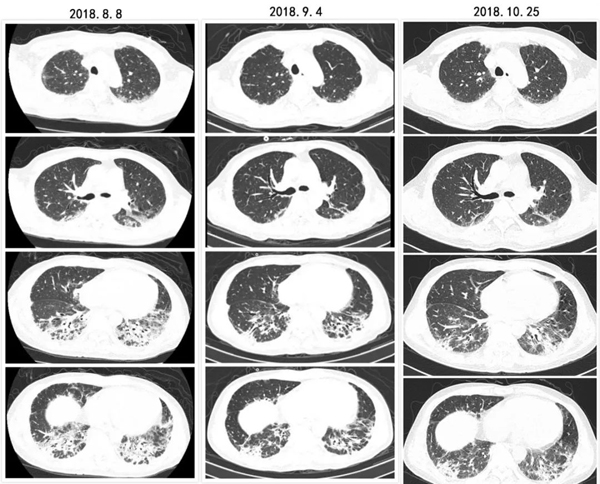
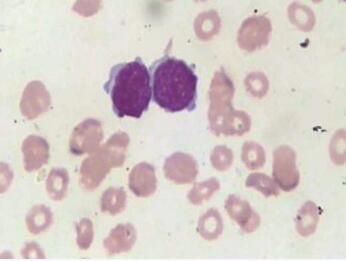
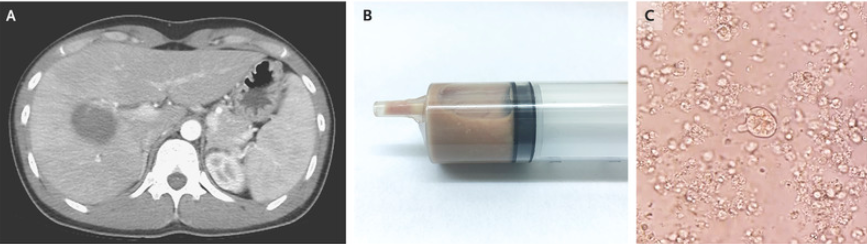
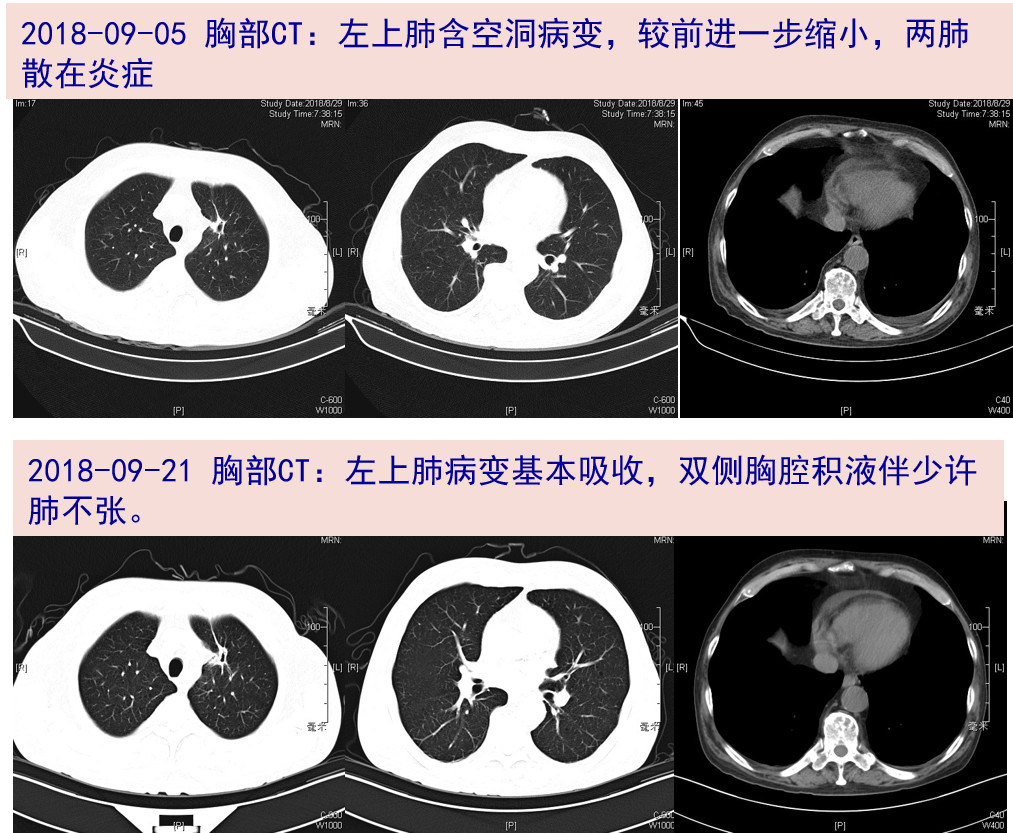
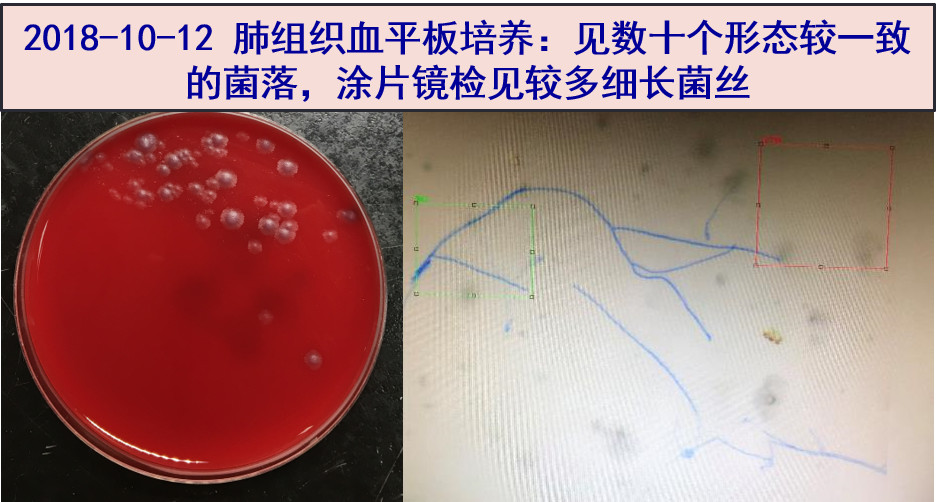
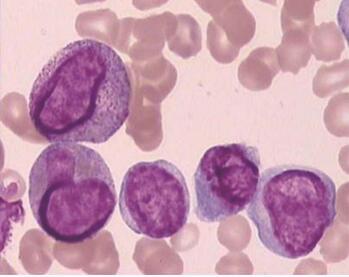
患者2周前受凉后出现咳嗽,干咳为主,偶少量白稀痰,伴发热(体温不详),曾于外院就诊,诊断“社区获得性肺炎”,予以抗感染治疗,症状无改善。1周前出现活动后气促,并呈进行性加重。遂转至当地人民医院住院治疗,胸部CT示“双肺间质病变并感染”,予“比阿培南+利奈唑胺”抗感染,症状无改善,现为求进一步诊治收住我科。起病以来,患者精神稍差,食纳及睡眠可,大小便正常,体重无明显变化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#间质性#
47
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
94
学习了长知识
88
学习了长知识学习了新知识
97
学习了新知识
82
学习了长知识
94
学习了新知识
30
学习了长知识
30
学习了新知识
26
学习了长知识
47