Gut:HBV患者血清dlDNA比例的增加与肝病的进展有关
2015-06-27 MedSci MedSci原创
Gut:HBV患者血清dlDNA比例的增加与肝病的进展有关HBV具有两种形式的基因组,松弛环状DNA(rcDNA)和复式线状DNA(dlDNA)。研究表明,与rcDNA相比,dlDNA更常见整合至宿主细胞染色体中,并有致癌的倾向。然而,相对于总的HBV DNA,dlDNA的比例以及其临床意义仍有待研究。基于 rcDNA 和dlDNA之间结构的差异,研究人员开发出一种肽核酸(PNA)介导的实时定量P
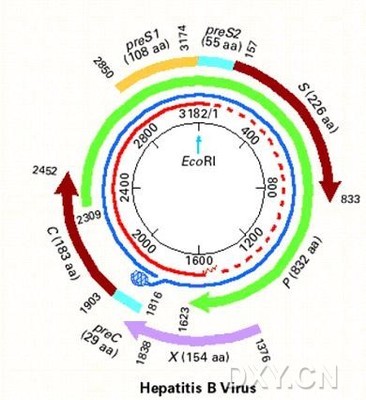
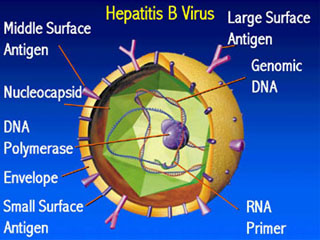
HBV具有两种形式的基因组,松弛环状DNA(rcDNA)和复式线状DNA(dlDNA)。研究表明,与rcDNA相比,dlDNA更常见整合至宿主细胞染色体中,并有致癌的倾向。然而,相对于总的HBV DNA,dlDNA的比例以及其临床意义仍有待研究。
基于 rcDNA 和dlDNA之间结构的差异,研究人员开发出一种肽核酸(PNA)介导的实时定量PCR(qPCR)钳夹方法,以检测慢性乙肝B(CHB)患者、肝硬化(LC)患者或LC基础上发展为肝细胞肝癌(HCC)的患者血清中dlDNA和总HBV DNA的比例。同时对影响dlDNA比例的因素进行研究。
结果发现,慢性HBV感染患者的血清中 dlDNA的平均比例约为7%,CHB患者中,dlDNA的比例随着丙氨酸转移酶的异常水平而增加。LC和HCC患者血清中dlDNA的比例分别约为14%和20%。干扰素-α治疗可使应答者的dlDNA比例轻度增加;核苷酸类似物治疗可使dlDNA的比例不合逻辑的升高。此外,体外研究表明,伴有炎症细胞因子升高的HBV复制可显著改变dlDNA的比例。
总而言之,该研究中,研究人员使用新型PNA介导的qPCR钳夹方法,首次发现了HBV相关性肝病发展过程中患者血清dlDNA的比例逐步增加。dlDNA的比例可受炎性因子的调节,表明验证中HBV dlDNA的比例增高可能与HCC的发生有关。
原始出处:
Zhao XL, Yang JR, Lin SZ, Ma H, Guo F, Yang RF, Zhang HH, Han JC, Wei L, Pan XB.Serum viral duplex-linear DNA proportion increases with the progression of liver disease in patients infected withHBV. Gut. 2015 Jun 4. pii: gutjnl-2014-308989. doi: 10.1136/gutjnl-2014-308989.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#HBV#
32
学习了,挺不错的
126
干扰素-α治疗可使应答者的dlDNA比例轻度增加;核苷酸类似物治疗可使dlDNA的比例不合逻辑的升高。?什么意思,那抗病毒治疗后dlDNA比例升高,意味着什么,肿瘤风险增高?
116
期待基于此而来的疾病新疗法
173
厉害
106
中国没有这种原创的创新的研究。
129
牛
73
o
99
哦
69