Lancet Respir Med:中国吸烟率与慢性病相关性研究
2018-10-26 MedSci MedSci原创
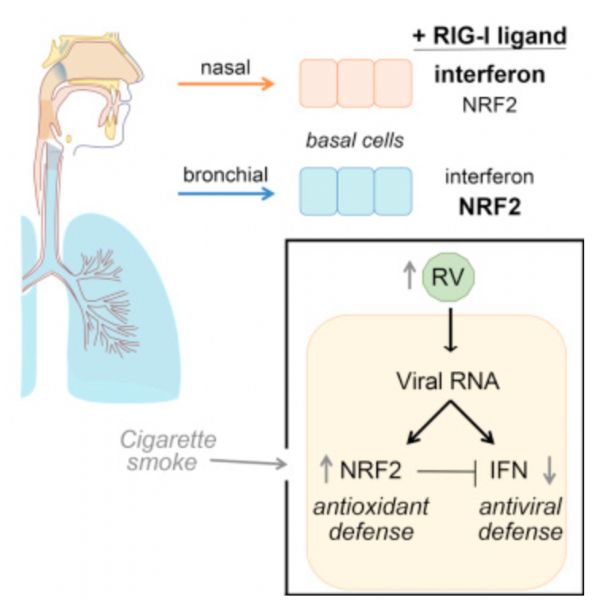
2003年世界卫生组织烟草控制框架公约签署以来,中国烟草控制政策未能有效降低中国人群的吸烟率,中国青少年人群及女性吸烟率大幅上升。研究认为需采取一定的措施,防止由于中国人口老龄化,与吸烟有关的慢性疾病负担进一步增加
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
51
#Lancet#
33
#相关性#
38
#慢性病#
42
#Med#
29
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
54