Drug Deliv:MMP10和BMP-2的组合可更好的促进骨再生
2018-03-13 MedSci MedSci原创
本研究对骨形态发生蛋白-2(BMP-2)和基质金属蛋白酶10(MMP10)的双重传送在骨再生中的效果在颅骨临界尺寸缺损的鼠模型进行了研究,假设它会增强骨形成。在小鼠中制备临界尺寸颅骨缺损(4mm直径),并且将预载有BMP-2、MMP10或两者的微球体组合的PLGA微球体以不同剂量移植到缺损部位。空微球体用作阴性对照。在14天内评估包囊效率并检测BMP-2和MMP10的体内释放动力学。4周和8周后使
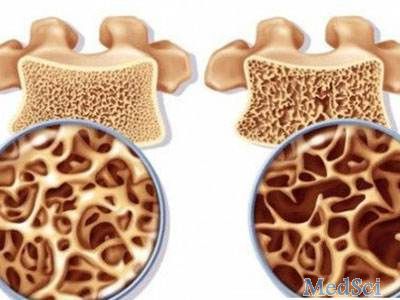
本研究对骨形态发生蛋白-2(BMP-2)和基质金属蛋白酶10(MMP10)的双重传送在骨再生中的效果在颅骨临界尺寸缺损的鼠模型进行了研究,假设它会增强骨形成。
在小鼠中制备临界尺寸颅骨缺损(4mm直径),并且将预载有BMP-2、MMP10或两者的微球体组合的PLGA微球体以不同剂量移植到缺损部位。空微球体用作阴性对照。在14天内评估包囊效率并检测BMP-2和MMP10的体内释放动力学。4周和8周后使用组织学分析来分析骨形成。
结果显示,与MMP10(30ng)的组合可明显增强BMP-2(600ng)-介导的骨生成。此外,通过用四环素和钙黄绿素进行双重标记测量现实,该组合还增加了矿物沉积速率(p <.05)。 MMP10通过增强BMP-2促进的骨愈合和改善矿化率来加速骨修复。
总之,MMP10和BMP-2的组合可能成为修复和再生骨缺陷的有前景的策略。
原始出处:
Reyes R, Rodríguez JA, et al., Combined sustained release of BMP2 and MMP10 accelerates bone formation and mineralization of calvaria critical size defect in mice. Drug Deliv. 2018 Nov;25(1):750-756. doi: 10.1080/10717544.2018.1446473.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Drug#
31
#BMP-2#
36
#BMP#
40
#骨再生#
30
不错的文章值得拥有
72
学习了.涨知识
54