经皮椎间孔镜手术治疗胸椎间盘突出症1例
2019-06-19 刘宇博 邹天明 中国骨与关节损伤杂志
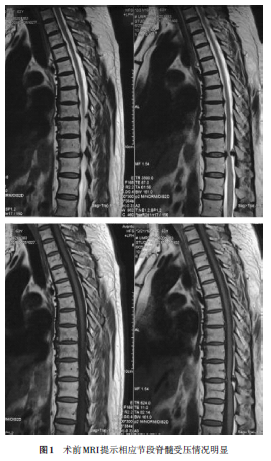
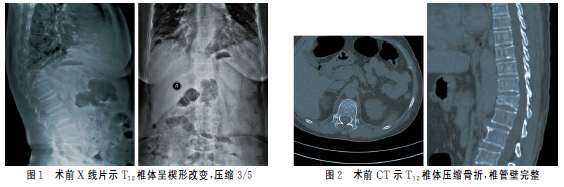
患者,男,50岁,因“左侧胸背部及左下肢疼痛、麻木半年余”入院。患者于半年前劳作后逐渐出现左侧胸背部及左大腿疼痛、感觉减退并伴有明显的下肢反射性疼痛,口服非甾体类消炎药后疼痛症状并未缓解,自觉对生活造成明显影响。入院查体:生命体征平稳,脊柱右侧呈现轻度侧弯姿态,胸腰部活动明显受限,胸腰段左侧有明显压痛、叩击痛,伴有左大腿前方感觉减退,叩击时可触发左大腿放射性疼痛,四肢肌力及肌张力未见明显增高,双侧

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#椎间盘突出#
30
#胸椎间盘突出症#
34
#椎间孔#
32
#椎间孔镜#
34
#手术治疗#
20
#胸椎#
25
谢谢了,学习
55
学习了很有用不错
50