专家共识│紧急抢救时ABO血型不相同血小板输注
2017-11-07 佚名 中国输血杂志
1965年AsteR提出血小板ABO不相容输注患者的血循环中血小板恢复程度低于同型输注的患者以来,血小板治疗性输注已有50 多年的历史,目前全世界每年的血小板输注量已达1000万U。
1965年AsteR提出血小板ABO不相容输注患者的血循环中血小板恢复程度低于同型输注的患者以来,血小板治疗性输注已有50 多年的历史,目前全世界每年的血小板输注量已达1000万U。
血小板相容性输注的国内外指南
我国卫生部2000年发布的《临床输血技术规范》中《成分输血指南》指出: 输注手工分离制备的浓缩血小板时应做交叉配血试验; 输注机采(单采) 浓缩血小板时应与ABO血型同型。其中并未涉及血小板ABO 相容性输注,但由于血小板资源匮乏、供应量有限、临床紧急输注的不确定性以及血小板保存期短、寻找1个与患者的HLA 和HPA相配和ABO相合的献血者相当困难等原因,在一些紧急或特殊情况下,要保证血小板ABO同型输注常遇到难以克服的困难。而国际上发达国家颁布的血小板输注指南中则基本包含了血小板的相容性输注规则,允许当ABO血型相合血小板供不应求时,可以输注ABO血型不同的血小板。
1英国血液学标准委员会颁布的《血小板输血指南》
建议在ABO同型血小板无法供应时,可接受ABO 血型不同的血小板; 将O 型血小板用于其他血型患者时,应做抗体检测,并确定不含有高效价的抗-A 和抗-B; 在输血实践中,输注ABO 不同型的血小板是可以接受的; 特别是当血小板供应匮乏、HLA 最佳匹配而ABO 血型不匹配时,可以使用ABO 不同型的血小板。检验医学网
2美国新英格兰地区《血液成分输注指南》
建议如果无法得到与ABO 血型相合的血小板,输注ABO 血型不同的血小板也能取得较好的临床效果; 在这种情况下,虽然同时输注了大量与ABO 血型不同的血浆,血浆白会导致受血者的抗球蛋白试验阳性,却罕见红细胞溶血反应的发生。
3美国《新生儿和婴儿血小板输注》
美国病理学家和AABB专家认为,紧急情况下的ABO不同型输注是安全的;就婴儿来说,没有ABO同型的血小板可供输注时,尽量选择血浆量少的不同型血小板,可以减少溶血发生的可能。
4英国《新生儿与儿童输血指南》
建议新生儿、小儿急性出血需要输注血小板时,应尽量选择血浆相容(即存在次侧相容)的血小板。由于A2亚型供血者的血小板表面基本不含A 抗原,其适合作为A 与O 型个体的血小板供血者,不仅有利于增高血小板储备量,而且便于HLA 相合血小板的选择。挪威已正式将A2亚型供血者定义为“万能血小板供者”。当O血型受(血)者接受ABO 血型非同型移植(输血)时,亦可输注A2亚型血小板。
ABO 血型不同的血小板输注分类
ABO血型不相同的血小板输注可以分为主侧ABO血型不相容的血小板输注、次侧ABO血型不相容的输注和同时存在主次侧不相容的输注3类。
推荐使用ABO血型不相同的血小板输注的原则
血小板输注应首选与受血者ABO 和RhD 血型同型血小板,由于血小板供应有限、保存期短和血小板输注的不确定性等因素,临床输血实践中,可以接受ABO 血型不相同的血小板输注。为减少人工分离制备的浓缩血小板中红细胞的输入,建议在输注ABO 血型不合血小板时使用单采血小板。
1哪些情况推荐使用ABO不同型的单采血小板输注
1)ABO同型血小板供应短缺、临床紧急需要血小板输注;
2)患者血型难以判断;
3)HLA 配型相合而ABO 血型不相合时,HLA 配型为首选。
2输注ABO 不同型的单采血小板注意事项
1)含高效价抗-A、抗-B的O型单采血小板输注给其他血型患者时可能引起溶血,建议使用抗-A、抗-B效价≤64 的O型单采血小板;但目前尚无公认的检测高效价抗-A、抗-B的试验方法,也无明确的实验室操作指南,临床使用时应予注意。
2)血小板表面缺乏Rh抗原,Rh阴性患者可输注Rh阳性的单采血小板,但应避免使用Rh阳性的浓缩血小板。
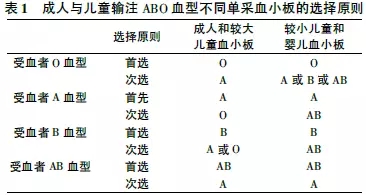
3成人和儿童输注ABO不同型单采血小板时推荐采用不同的规则
1)成人和较大儿童(建议≥6 岁)采用主侧相容的ABO不同型单采血小板;
2)较小儿童(建议<6 岁)和婴儿采用次侧相容的ABO不同型单采血小板( 表1) 。
4接受ABO 血型不同的单采血小板输注前告知事项
使用ABO血型不同的单采血小板输注,具有一定止血效果,但同时存在一定风险,必须告知患者或监护人,风险包括但不限于:
1)血小板输注无效可能,无法起到止血效果。
2)供者血浆中存在的ABO 血型抗体可能引起急性溶血反应,如发热、腹痛、尿色深、红等; 也有可能引起抗球蛋白试验阳性。
3)其他与同型输注一样的输血风险,如感染、HIV、梅毒、传染性肝炎等。
ABO血型不同的单采血小板输注指证
在紧急抢救患者生命,必须接受血小板输注治疗时,如因客观条件所限,患者无法输注ABO同型血小板而必须接受ABO不同型输注时,其输注指征同接受ABO同型的血小板输注指征。
ABO血型不同的单采血小板输注禁忌症
此禁忌证与接受ABO 同型血小板输注禁忌症相同。
1血栓性血小板减少性紫癜(TTP)
1)血小板输注可促进血栓形成,加重病情;
2)患者只有在有威胁生命的出血发生时,才可输注血小板,否则不应输注任何血小板制剂。
2肝素诱导血小板减少症(HIT)
是药物诱导的免疫性血小板减少症,输注血小板可导致急性动脉血栓,不宜输注血小板。
3特发性血小板减少性紫癜( ITP)
患者体内存在的血小板自身抗体不仅可以破坏自身和大多数供者的血小板,而且还阻碍自身血小板的生成。输入的血小板在ITP患者体内存活时间明显缩短,甚至发生ITP患者输注血小板后的血小板计数不升反降,故ITP患者不可能用输注血小板来达到血小板计数的提高。ITP患者只有在下列情况下才可输注血小板:
1)脾切除治疗手术前或手术过程中发生严重、不可控制的出血;
2)Plt<20×109/L并伴有严重出血,可能危及生命。
ABO 血型不同的单采血小板输注后疗效评估
此评估方法与接受ABO 同型血小板输注后疗效评估相同。目前临床判断的依据主要有血小板恢复百分率( PPR) 和输注后血小板计数纠正增加指数(CCI) 以及患者临床出血状况的改善。血小板输注后患者出血症状改善程度不易量化,故以PPR 和CCI 作为量化的判断依据。
1PPR计算公式
PPR(%) = ( 输后Plt-输前Plt) ×血容量( L) /输注血小板总数×2/3。输注后1h 30%<PPR<60%或输注后24h 20%<PPR<50%,为输注有效; 输注后1h PPR<30%或输注后24h 的PPR<20%,为输注无效。
2CCI 计算公式
CCI = (输后Plt-输前Plt) × 体表面积(m2)/输入血小板总数( × 1011)[体表面积= 0. 0061×身高(cm) +0. 0128×体重(kg)-0.1529]; 输注后1h CCI>7. 5×109/L或输注后24h CCI>4.5×109/L为输注有效。
ABO 血型不同的单采血小板输注后监测
接受ABO 血型不同的单采血小板输注,具有一定风险,输注前后可监测但不限于以下指标: 血清总胆红素、血清间接胆红素、血清游离血红蛋白、尿胆红素、直接抗球蛋白试验等。其他监测指标与同型单采血小板输注相同。
临床输血实践证明输注ABO 血型不相同的单采血小板
对于挽救急性血小板减少引起的危及生命的出血患者可以取得良好的临床效果。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#紧急抢救#
40
#专家共识#
30
#血小板输注#
38
#ABO血型#
45
#抢救#
36
#紧急#
26
#ABO#
29
很好的文章.谢谢分享!
0
学习一下谢谢分享
59