Lab Invest:视网膜相关孤核受体α(RORα)缺陷表现出睾丸形态缺陷
2019-08-27 AlexYang MedSci原创
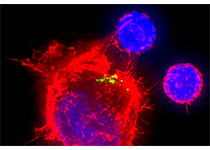
视网膜相关孤核受体(已报道的睾丸中转录因子)在睾丸功能中的作用仍旧不清楚。最近,有研究人员在RORα缺陷小鼠中,使用光学、电子显微镜和免疫组化染色对睾丸结构的变化进行了定性和定量分析。研究发现,变异小鼠睾丸中最为明显的变化包括生殖功能低下,间质组织体积比例和间质细胞数量明显减少,生精管直径和上皮高度显著减少,生精小管上皮空泡化,肥大细胞出现,精子出现延迟征象以及精子形态发生变化。更多的是,突变小鼠
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EST#
34
#核受体#
39
#视网膜#
32
#睾丸#
36