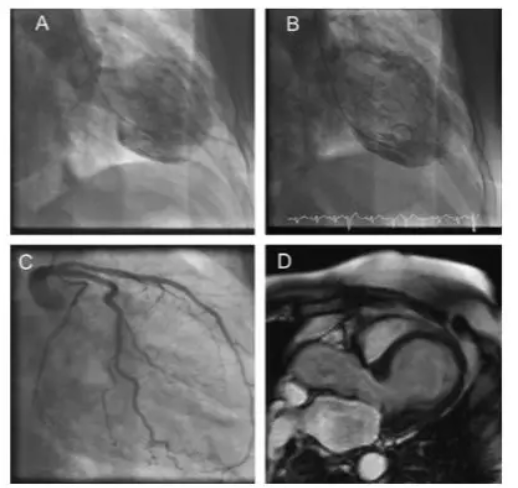
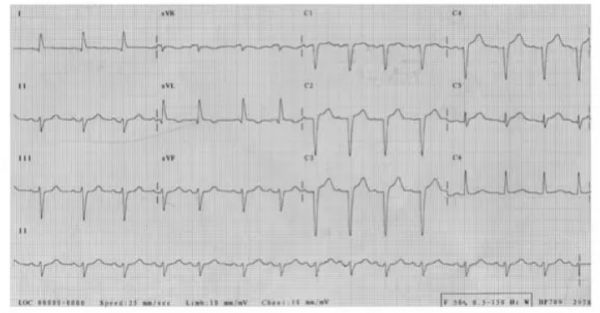
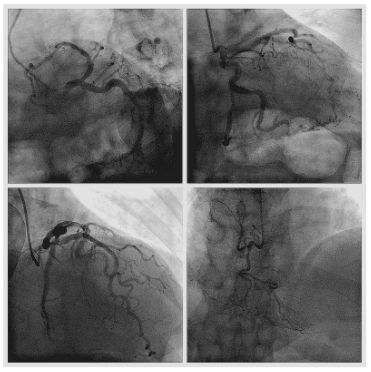
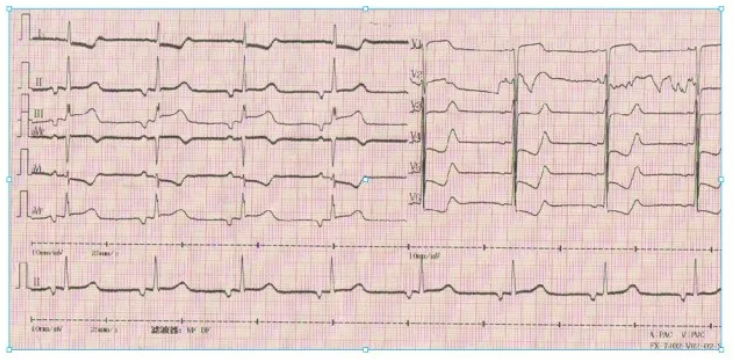
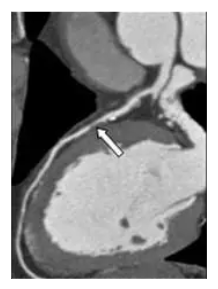
病例分享:胸痛+ST段抬高+肌钙蛋白升高,不一定就是心梗!
2018-04-24 人间世 医学界心血管频道
骑白马的不一定是唐僧,还可能是我们心目中万分期待的王子。因此,当胸痛+ST段抬高+肌钙蛋白(cTn)升高找上门时,其背后的元凶也许并不十分可怕,而是急性心梗的“最善意的模仿者”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ST段抬高#
25
#ST段#
25
好文章.学习了
76
学习了.谢谢分享
69
很好的病历.确实提供另外一种思路
71
了解一下.谢谢分享!
70
^_^^_^^_^
67
可以学习
19