Blood:维奈托克联合利妥昔单抗±苯达莫司汀治疗复发性/难治性滤泡性淋巴瘤
2020-08-27 MedSci原创 MedSci原创
CONTRALTO试验是一个开放标签的2期研究,旨在评估BCL-2抑制剂维奈托克(VEN)联合利妥昔单抗(R),VEN联合苯达莫司汀(B)和R,对比单用BR治疗复发性/难治性滤泡性淋巴瘤的疗效和安全性

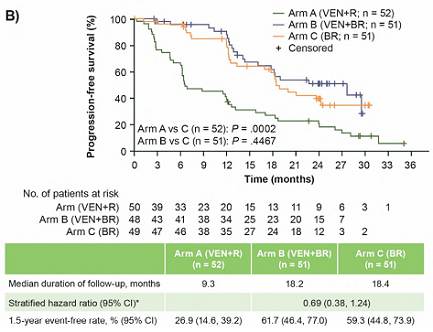
与C组相比,B组更频繁的血液毒性导致给药剂量减少或停药。A、B、C组3/4级不良反应发生率分别是51.9%、93.9%和60.0%。与C组相比,VEN+BR的毒性增加,用药剂量减少,但疗效相似。
优化剂量和方案以维持苯达莫司汀和利妥昔单抗的剂量强度或可提高VEN联合苯达莫司汀和利妥昔单抗的疗效和耐受性,而VEN联合利妥昔单抗的数据有待进一步研究。
原始出处:
Pier Luigi Zinzani,et al. Venetoclax-rituximab ± bendamustine vs bendamustine-rituximab in relapsed/refractory follicular lymphoma: CONTRALTO. Blood. August 12,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性#
37
#利妥昔#
29
#滤泡性淋巴瘤#
50
#难治性#
39
#苯达莫司汀#
40
学习了
111
已读
97
值得我们学习#学习##学习#
116
很好
119