Clinica Chimica Acta:新型PHI诺模图的开发和内部验证以识别侵袭性前列腺癌
2020-03-19 MedSci原创 MedSci原创
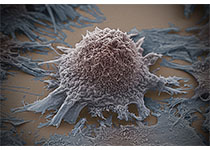
前列腺健康指数(PHI)是一种新的前列腺癌(PCa)检测方法,提高了总PSA (tPSA)的表现,并与肿瘤的侵袭性有关。本研究目的是在包含PHI的多变量模型的基础上构建诺模列线图。
前列腺健康指数(PHI)是一种新的前列腺癌(PCa)检测方法,提高了总PSA (tPSA)的表现,并与肿瘤的侵袭性有关。本研究目的是在包含PHI的多变量模型的基础上构建诺模列线图,以估计侵袭性PCa的个体可能性。
研究人员选择了276名活检对象,其中包括151名PCa患者。采用D 'Amico标准将这些患者分为三组,这三组与进展风险相关。将中度和高危PCa认为是侵袭性PCa。利用实验室(tPSA、%fPSA、%p2PSA、PHI)和临床变量建立了预测侵袭性PCa的多变量模型。以临床使用的列线图表示最佳预测模型以图形形式。
研究结果显示,年龄、直肠指检、tPSA、%fPSA、PHI、前列腺体积等多变量模型的准确性最高(AUC: 0.815)。DCA证实了诺模列线图的有效性,与包括年龄、直肠指检和tPSA的基础模型相比,其临床净获益(大于7%)更高。
研究结果表明,基于PHI诺模图是检测侵袭性PCa的有效工具。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CTA#
32
#侵袭性#
23
#诺模图#
24
前列腺癌相关研究,学习了,谢谢梅斯
33