Am J Neurodegener Dis:研究者发现肌萎缩性侧索硬化症治疗新靶点
2012-06-09 T.Shen 生物谷
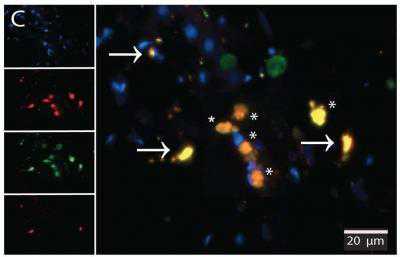
在ALS病人的脊髓中,病人的吞噬细胞(绿色)影响神经元(活的神经元是红色的,用星号标记;死的神经元,用品红标记的) (Credit: University of California, Los Angeles) 早期研究中,加州大学洛杉矶分校的研究者发现肌萎缩性侧索硬化症(ALS)病人的免疫细胞可能在破坏脊髓神经元上发挥着重要的作用。ALS是大脑和脊髓神经元细胞控制肌肉随意移动的疾

在ALS病人的脊髓中,病人的吞噬细胞(绿色)影响神经元(活的神经元是红色的,用星号标记;死的神经元,用品红标记的)
(Credit: University of California, Los Angeles)
早期研究中,加州大学洛杉矶分校的研究者发现肌萎缩性侧索硬化症(ALS)病人的免疫细胞可能在破坏脊髓神经元上发挥着重要的作用。ALS是大脑和脊髓神经元细胞控制肌肉随意移动的疾病。研究者发现ALS病人免疫系统引发的炎症可以触发吞噬细胞发挥功能。在炎症过程中,运动神经元会被吞噬细胞清除掉。
研究小组发现一种名为resolvin D1的脂质介质(在机体中由欧米伽3脂肪酸DHA组成)可以关闭炎症反应,炎症反应使得吞噬细胞对神经元具有很大的威胁性。resolvin D1可以封锁吞噬细胞产生的炎症蛋白,切断炎症反应过程。而且相比其它亲缘分子,resolvin D1可以像IL-6一样抑制关键的炎症蛋白,频率高达1100次以上。研究表明,DHA在中风病人和阿尔茨海默尔病人中起到了保护神经系统的作用。
研究者的这项最新研究中,他们从ALS病人和对照组的血液样品中分离到了吞噬细胞,并且从已故的捐献者体内分离出了脊髓细胞。这项研究揭示了,resolvin D1的发现为减弱ALS病人的炎性反应提供了思路。但是当前研究者并没有有效的方法用resolvin给病人给药,因此resolvin D1用于病人的治疗还需要一段时间。尽管DHA在临床试验中并没有检测其对ALS病人的效应,但是目前研究者已经将DHA用于阿尔兹海默病病人、中风病人以及脑损伤病人的治疗过程中。相关研究成果刊登在了国际杂志American Journal of Neurodegenerative Disease上。(生物谷Bioon.com)
编译自:How Immune System, Inflammation May Play Role in Lou Gehrig's Disease
编译者:T.Shen

PMC:
PMID:
Neuronal phagocytosis by inflammatory macrophages in ALS spinal cord: inhibition of inflammation by resolvin D1
Guanghao Liu, Milan Fiala, Mathew T Mizwicki, James Sayre, Larry Magpantay, Avi Siani, Michelle Mahanian, Madhuri Chattopadhay, Antonio La Cava, Martina Wiedau-Pazos
Although the cause of neuronal degeneration in amyotrophic lateral sclerosis (ALS) remains hypothetical, there is evidence of spinal cord infiltration by macrophages and T cells. In post-mortem ALS spinal cords, 19.8 + 4.8 % motor neurons, including caspase–negative and caspase-positive neurons, were ingested by IL-6- and TNF-α-positive macrophages. In ALS macrophages, in vitro aggregated superoxide dismutase-1 (SOD-1) stimulated in ALS macrophages expression of inflammatory cytokines, including IL-1β, IL-6, and TNF-α, through activation of cyclooxygenase-2 (COX-2) and caspase-1. The lipid mediator resolvin D1 (RvD1) inhibited IL-6 and TNF-α production in ALS macrophages with 1,100 times greater potency than its parent molecule docosahexaenoic acid. ALS peripheral blood mononuclear cells (PBMCs) showed increased transcription of inflammatory cytokines and chemokines at baseline and after stimulation by aggregated wild-type SOD-1, and these cytokines were down regulated by RvD1. Thus the neurons are impacted by macrophages expressing inflammatory cytokines. RvD1 strongly inhibits in macrophages and PBMCs cytokine transcription but does not inhibit their production in PBMCs. Resolvins offer a new approach to ALS inflammation suppressing. (AJND1103001)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#萎缩性#
29
#Gene#
36
#萎缩#
33
#硬化症#
35
#Dis#
25
#研究者#
25
#新靶点#
25
#肌萎缩#
25
#治疗新靶点#
33