Lancet Oncology:帕唑帕尼为成人进展型硬纤维瘤带来一线希望
2019-08-07 佚名 肿瘤资讯
硬纤维瘤是一类罕见、局部侵袭性肿瘤,关于这类患者的系统性治疗方案非常有限,甲氨蝶呤联合长春花碱化疗是唯一一个经过临床试验验证的方案。近日发布在Lancet Oncology杂志的DESMOPAZ研究,在进展型硬纤维瘤患者中评估帕唑帕尼和甲氨蝶呤联合长春花碱治疗的疗效和安全性。
背景
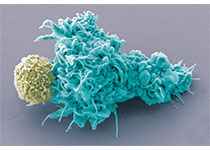
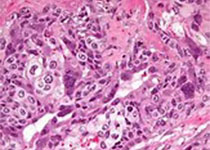
硬纤维瘤是一类罕见、局部侵袭性肿瘤,疾病进程很难预测,多见于15~60岁人群。几十年来,手术切除一直是这类患者的标准治疗模式,研究提示诊断后一线采用单纯观察模式,无需其余治疗,患者同样可以获益。然而,约1/3的硬纤维瘤侵袭性较强或合并一定的症状,需要干预处理。既往一些相关的药物探索,如激素治疗(如他莫昔芬)、非固醇类抗炎药物(NSAIDs)、TKI(如伊马替尼或索拉非尼)和细胞毒性化疗,用于进展或复发型硬纤维瘤患者,均取得了一定临床获益。然而,这些系统性治疗的研究证据非常有限,且均是基于小样本量的单中心研究。甲氨蝶呤联合长春花碱化疗是唯一一个经过临床试验验证的系统性治疗方案,显示出有前景的疗效,安全性可耐受,尤其是用于儿童、青少年和年轻人群。研究发现硬纤维瘤常高表达VEGF,尤其是在复发、侵袭性疾病中。回顾性数据显示,26例接受索拉非尼治疗的硬纤维瘤患者显示出有前景的疗效。帕唑帕尼是一个靶向VEGFR1、2、3、PDGFRα、β和c-KIT的TKI,目前已经获批用于软组织肉瘤治疗。本研究旨在进展型硬纤维瘤患者中评估帕唑帕尼和甲氨蝶呤联合长春花碱治疗的疗效和安全性。
方法
DESMOPAZ是一项非对比、随机、开放、多中心二期研究,从法国肉瘤协作组12个研究中心招募患者。入组年龄18岁或以上,组织学确诊的硬纤维瘤,ECOG PS 0~1分。重要排除标准包括既往接受过帕唑帕尼或甲氨蝶呤联合长春花碱治疗。符合入组标准的患者按2:1随机分配接受帕唑帕尼或甲氨蝶呤联合长春花碱治疗,分层因素包括研究中心和肿瘤部位(四肢和腰部 vs 其他)。两组患者分别接受帕唑帕尼治疗1年或甲氨蝶呤联合长春花碱治疗每周用药6个月序贯每2周用药6个月,治疗直至疾病进展或不可耐受的毒性或研究者决定停药或患者要求出组,至多治疗1年。主要研究终点为6个月未出现疾病进展的患者比例,次要研究终点为安全性、最佳疗效、1年和2年的PFS率、OS和生活质量。
结果
2012年12月4日至2017年8月18日,共72例患者参与随机。在随机后,甲氨蝶呤联合长春花碱组2例患者排除本研究(1例要求出组,1例既往接受过帕唑帕尼治疗),最终70例患者接受治疗。入组患者的中位年龄为40岁,2/3为女性。总体人群中,3/4的患者既往接受过系统性治疗,中位治疗线数为一线。
患者的中位随访时间为23.4个月,帕唑帕尼组和甲氨蝶呤联合长春花碱组分别有52%(25/48)和23%(5/22)的患者完成了1年治疗。治疗终止的主要原因为疾病进展(两组分别为13%和27%)、不可耐受的毒性(8%和23%)和其他原因(2%和14%)。8例患者在治疗进展后接受交叉治疗:帕唑帕尼组2例交叉接受甲氨蝶呤联合长春花碱;甲氨蝶呤联合长春花碱组6例交叉接受帕唑帕尼治疗。4例患者无法进行疗效评估,最终66例患者纳入疗效分析:帕唑帕尼组中最初入组的43例可评估患者中,36例患者在6个月时仍未出现进展,6个月的无进展率为83.7%;甲氨蝶呤联合长春花碱组中6个月的无进展率为45.0%。两组的中位PFS均尚未达到。帕唑帕尼组1年和2年的PFS率分别为85.6%和67.2%;甲氨蝶呤联合长春花碱组均为79.0%。
疗效分析
截至本次分析,除帕唑帕尼组中1例患者死亡以外,其他患者均存活,两组的中位OS均尚未达到,2年、3年和4年的OS率相似,帕唑帕尼组和甲氨蝶呤联合长春花碱组分别为97.3%和100%。在帕唑帕尼组中,大多数的患者出现肿瘤缩小,见图1C;46例患者中,17例(37.0%)取得PR,27例(58.7%)取得SD,2例(4.4%)为PD(其中1例合并加德纳氏综合征,1例为CTTNB1野生型肠系膜肿瘤)。甲氨蝶呤联合长春花碱组的20例患者中,11例(55%)观察到肿瘤缩小,见图1D;5例(25%)患者最佳疗效为PR,10例(50%)为SD,4例(20%)为PD,见。
安全性分析
70例患者可进行安全性分析,帕唑帕尼组和甲氨蝶呤联合长春花碱组3-4度不良事件(AE)发生率分别为56%和77%;两组最常见的3-4度AE,帕唑帕尼组为高血压和腹泻;甲氨蝶呤联合长春花碱组为中性粒细胞减低和转氨酶升高。
生活质量评估
帕唑帕尼组基线和治疗第6个周期的总体生活质量评分稳定,疼痛强度有所减低;甲氨蝶呤联合长春花碱组治疗第6周期的总体生活质量评分较基线降低10分以上,且情感功能评分也出现有临床意义的降低。
探索性分析
共28例患者有足够的肿瘤组织标本进行蛋白组学分析,其中帕唑帕尼组和甲氨蝶呤联合长春花碱组分别为21例和7例。根据RECIST标准评估的肿瘤缩小比例将帕唑帕尼组患者分为3组,聚类分析显示,取得客观缓解的患者对比治疗无响应的患者,蛋白表达谱存在显着差异。
结论和讨论
在硬纤维瘤这类罕见的肿瘤中进行随机临床研究是非常具有挑战的,DESMOPAZ研究是第一项在确认进展的硬纤维瘤患者中进行的非对比的随机研究,3/4的入组患者既往接受过系统性治疗且在治疗6个月内出现疾病进展。本研究结果显示,患者接受帕唑帕尼治疗,6个月的未进展率为83.7%,研究达到主要终点。这一研究结果证实,帕唑帕尼用于进展型硬纤维瘤显示出一定的临床疗效,可以考虑作为这类罕见疾病的治疗选择。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬纤维瘤##帕唑帕尼#
51
#Oncol#
31
#Oncology#
25
#Lancet#
28
#成人进展型#
30
#纤维瘤#
35
#硬纤维瘤#
30
谢谢梅斯分享这么多精彩信息
37