CSCO 2016:北大肿瘤医院专家解读左右半结肠癌
2016-09-29 MedSci MedSci原创
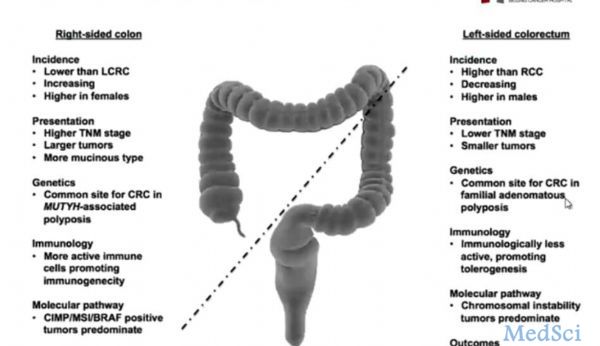
左右半结肠癌是两种不同的疾病 1、左右半结肠癌临床表现不同 2、左右半结肠癌病理分型不同:分化差/粘液腺癌/印戒细胞癌 右半>左半 3、左右半结肠胚胎起源不同: 4、左右半结肠微生物环境不同:结直肠癌组织中核粒梭形杆菌DNA量与较差的生存相关,有可能是预后因素。5、左右半结肠免疫环境不同:右半结肠PD-L1和P
2016年9月22日-24日,第19届全国临床肿瘤学大会暨2016年CSCO学术年会在福建厦门国际会议中心举行。北京大学肿瘤医院消化肿瘤内科沈琳教授做了题为“不同部位结肠癌生物学特性和治疗决策”的报告,梅斯小编对其精彩内容进行整理与大家分享。
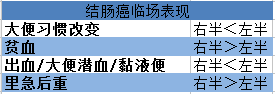
2、左右半结肠癌病理分型不同:
分化差/粘液腺癌/印戒细胞癌 右半>左半
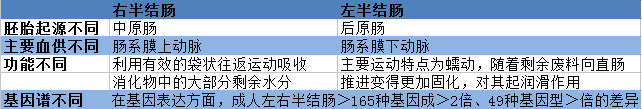
3、左右半结肠胚胎起源不同:
3、左右半结肠胚胎起源不同:
4、左右半结肠微生物环境不同:结直肠癌组织中核粒梭形杆菌DNA量与较差的生存相关,有可能是预后因素。
5、左右半结肠免疫环境不同:右半结肠PD-L1和PD-1的表达均高于左半结肠癌
6、左右半结肠癌预后不同
2016你那SEER分析显示:在Ⅲ/Ⅳ期患者中,右半结肠癌的生存期显著低于左半结肠癌,而左半结肠癌与直肠癌预后相似。
7、左右半结肠癌差异终归结于分子层面的不同
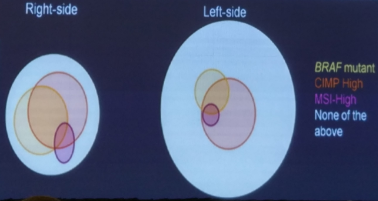
左右半结直肠癌的分子病理分型不同-CMS
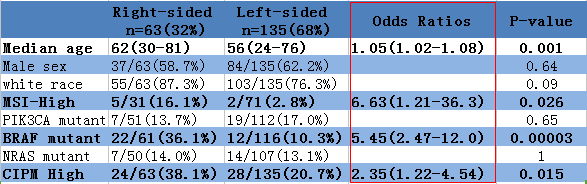
由上表可知:右半结肠的BRAF突变率高,甲基化率高,MSI-H比例高
左右半结肠的临床病理及分子生物学特征
肿瘤原发部位可能是化疗的预测因素ORR :43%(左)vs 37%(右);p=034
另外,右半结肠粘液腺癌比例高,可能对化疗反应差。右半结肠是预后差的因素,bevacizumab的疗效与肿瘤部位无关。对于KRAS野生型的患者,肿瘤部位可能是cetuximab疗效的预测因素,左半结肠患者PFS及mOS均长于右半结肠。KRAS野生型的难治性肠癌中, 左半结肠癌接受cetuximab治疗较右半结肠能获得更好的PFS。左半结肠接受FOLFIRI+cetuximab治疗比FOLFIRI+bevacizumab能获得更好的OS。
那么,对于左半结肠癌RAS野生型患者,EGFR单抗是否是一线治疗的优选方案?
沈琳教授解答说,就OS而言,EGFR单抗可作为左半结肠癌的一线治疗优选方案,但是治疗决策需结合患者年龄、PS评分、基础疾病、原发灶情况、生活质量等综合评估,全程管理患者。
右半结肠RAS野生型是否初始治疗就不推荐选用EGFR单抗?
沈琳教授解答说,可不选用
右半结肠癌预后差,对化疗和靶向治疗反应率第,是否有别的治疗手段?
沈琳教授说,可能有。
1.多靶点抑制BRAF通路?
2.免疫治疗?
3.MEK抑制剂?
9、右半结肠癌未来可能的治疗手段
(1)BRAF突变率高,可否三药抑制BRAF通路?
1项多中心Ⅱ期药物临床试验(Clinical Trials,NCT01719380):
BRAF抑制剂+EGFR单抗(50例)vs BRAF抑制剂+EGFR单抗+PI3K抑制剂(52例),结果发现ORR 22% vs 27%,PFS 4.2mos vs 5.4 mos
(2)MSI-H比例高用PD-1治疗?
(3)PD-1/PD-L1抗体在微卫星稳定(MSS)的CRCs患者中的有效率较其他适应症偏低,MEK靶向抑制会导致MHC I 对肿瘤细胞作用上调,诱导瘤内T-细胞浸润同时增强抗-PD-L1活性,并同时抑制KRAS下游通路。这对于MARK信号通路活跃的右半结肠癌是否会是新的治疗手段呢?
10、总结:
(1)流行病学存在差异:左半高发,然而呈现下降趋势,多见于男性;右半相对低发,但呈上升趋势,多见于女性。
(2)胚胎来源和解剖结构均有所不同。
(3)微生物及免疫环境不同。
(4)分子病理分型不同:右半病理类型常见粘液腺癌,有高度的微卫星不稳定性、BRAF突变,突变事件丰富,CMS分型为1,3型;左半则存在染色体不稳定和非整倍体现象,突变事件相对不丰富,CMS分型为2,4型。
(5)原发病灶的解剖部位与预后相关,也可能与药物治疗效果有关。
(6)右半结肠癌分子事件较多,针对这些分子事件,未来可能应用新的治疗手段。
2.免疫治疗?
3.MEK抑制剂?
9、右半结肠癌未来可能的治疗手段
(1)BRAF突变率高,可否三药抑制BRAF通路?
1项多中心Ⅱ期药物临床试验(Clinical Trials,NCT01719380):
BRAF抑制剂+EGFR单抗(50例)vs BRAF抑制剂+EGFR单抗+PI3K抑制剂(52例),结果发现ORR 22% vs 27%,PFS 4.2mos vs 5.4 mos
(2)MSI-H比例高用PD-1治疗?
(3)PD-1/PD-L1抗体在微卫星稳定(MSS)的CRCs患者中的有效率较其他适应症偏低,MEK靶向抑制会导致MHC I 对肿瘤细胞作用上调,诱导瘤内T-细胞浸润同时增强抗-PD-L1活性,并同时抑制KRAS下游通路。这对于MARK信号通路活跃的右半结肠癌是否会是新的治疗手段呢?
10、总结:
(1)流行病学存在差异:左半高发,然而呈现下降趋势,多见于男性;右半相对低发,但呈上升趋势,多见于女性。
(2)胚胎来源和解剖结构均有所不同。
(3)微生物及免疫环境不同。
(4)分子病理分型不同:右半病理类型常见粘液腺癌,有高度的微卫星不稳定性、BRAF突变,突变事件丰富,CMS分型为1,3型;左半则存在染色体不稳定和非整倍体现象,突变事件相对不丰富,CMS分型为2,4型。
(5)原发病灶的解剖部位与预后相关,也可能与药物治疗效果有关。
(6)右半结肠癌分子事件较多,针对这些分子事件,未来可能应用新的治疗手段。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肿瘤医院#
25
#专家解读#
26
文章很好,继续关注
49
学习了!谢谢!
60
继续关注!
55
谢谢分享!
58