JAHA:一种新的单叶主动脉瓣小鼠模型
2018-07-01 MedSci MedSci原创
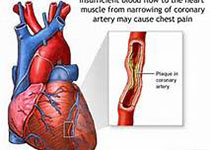
既往研究报道上皮生长因子受体家族可以调控胚胎的半月瓣膜发育,本研究的目的旨在探索上皮生长因子受体的杂合显性突变小鼠模型EgfrVel/+的半月瓣形态变化。本研究对2.5-4个月大小的EgfrVel/+小鼠和对照小鼠的主动脉瓣进行了体视显微镜观察,并在2.5、4.5、8和12个月对EgfrVel/+小鼠和对照小鼠进行了超声心动图检查和病理组织学检测。分析结果显示,79%的EgfrVel/+小鼠主动脉
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AHA#
41
#主动脉瓣#
45
#主动脉#
0
#小鼠模型#
48
学习了.获益匪浅.感谢分享.收藏了
78
学习了.长知识
78