NAT STRUCT MOL BIOL :许琛琦组等揭示T细胞共刺激受体CD28的活性调控机制
2017-10-24 BioArt BioArt
CD28是T细胞中关键的共刺激受体,它调控T细胞的发育、分化、代谢、迁移等生理过程。近期研究还表明CD28可能成为肿瘤免疫治疗的一个重要分子标记。然而目前关于抑制CD28与下游分子产生自动结合的分子机制并不清楚,另外CD28的信号转导具有T细胞抗原受体依赖性激活的分子机理也不清楚。10月23日,中科院生物化学与细胞生物学研究所许琛琦研究组与牛津大学Omer Dushek研究组合作在Nature S
论文解读:
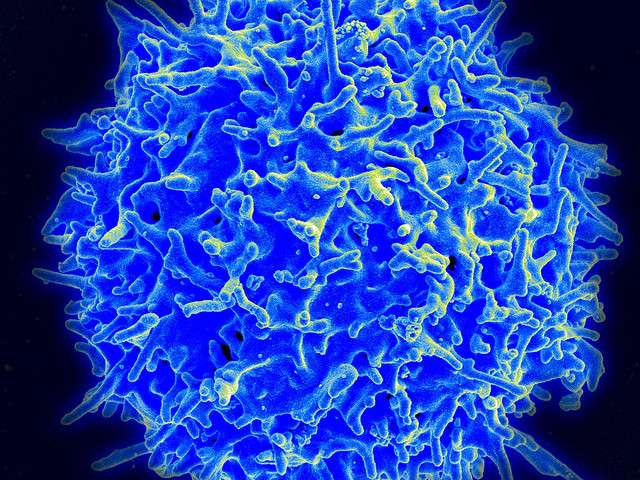
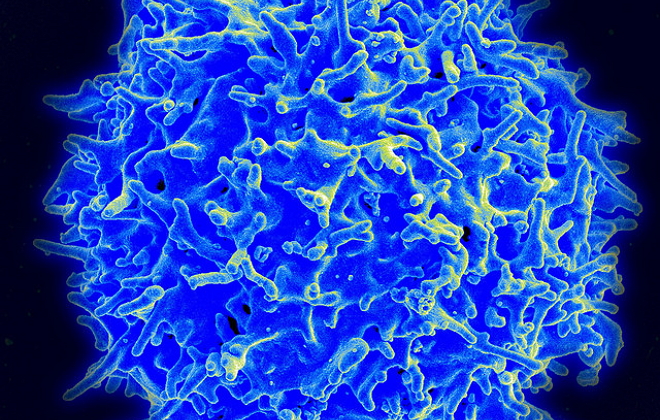
T细胞的完全活化依赖于T细胞抗原受体(T-cell receptor, TCR)提供的抗原刺激信号和共刺激受体提供的共刺激信号。CD28是T细胞中关键的共刺激受体,它调控T细胞的发育、分化、代谢、迁移等生理过程。针对CD28的阻断药物已经在临床上用于治疗自身免疫病和器官移植。近期研究表明PD-1主要是通过抑制CD28的信号转导来下调T细胞的肿瘤免疫应答反应,因此CD28可能成为肿瘤免疫治疗的一个重要分子标记。
CD28的信号转导依赖于其胞内区的41个氨基酸残基,其中含多个酪氨酸磷酸化位点和脯氨酸信号模体,能与PI3K,Grb2,Lck等下游分子产生磷酸化依赖或者磷酸化非依赖的相互作用。目前关于抑制CD28与下游分子产生自动结合的分子机制并不清楚。另外CD28的信号转导具有TCR依赖性,即只有存在TCR信号的时候,CD28才能被活化并激活相对特异的下游信号通路。这种信号依赖性的分子基础是什么也是个悬而未决的问题。
许琛琦研究组此前一直从事脂质分子调控T细胞功能的分子机制研究,前期的研究发现细胞质膜内层酸性磷脂通过与TCR/CD3胞内区碱性氨基酸发生静电相互作用从而屏蔽TCR的活化,而T细胞初始激活产生的Ca2+可通过静电竞争解除TCR的屏蔽并促进其磷酸化。
在对CD28跨膜信号转导的分子机制的研究中,许琛琦研究组利用生物化学、核磁共振和荧光成像技术发现CD28的胞内区能通过其碱性氨基酸富集区(Polybasic Region,PBR)与酸性磷脂发挥静电相互作用,将CD28胞内区完全地屏蔽在膜脂双层中,从而阻止了CD28与下游信号分子的自动结合。
随后许琛琦研究团队利用高分辨率钙成像发现TCR活化后会引发Ca2+在CD28周围的富集,这些钙离子能够通过静电竞争来直接打破CD28与酸性磷脂的静电相互作用,从而帮助CD28的活化,该发现解释了CD28对TCR依赖的信号机制和分子基础。结合TCR方面的研究成果,牛津大学Omer Dushek研究组利用数据建模的方法模拟了TCR与CD28的信号转导网络,提出了TCR-Ca2+-CD28所组成的正反馈调控环路可以迅速放大T细胞信号强度(下图),从而极大地提高T细胞的抗原响应敏感性。
TCR-Ca2+-CD28的正反馈环路模型
在静息状态下,带负电荷的酸性磷脂可以屏蔽TCR和CD28的活性位点;生理条件下,抗原的数量非常微量,抗原对TCR的初始激活可以诱发Ca2+内流;内流的Ca2+通过静电竞争解除TCR和CD28的活性位点,促进它们的信号转导;TCR和CD28的信号转导都可以进一步引起Ca2+内流。TCR-Ca2+-CD28之间由此形成了正反馈环路,可以迅速放大抗原刺激信号,从而为T细胞产生高抗原敏感性提供信号基础。胞内的Ca2+浓度还受钙转运蛋白的负调控,因此被维持在一个合理的水平,其生理功能主要包括短期的T细胞停止信号和长期的转录调控。
该论文的另一个亮点是预测了可能被酸性磷脂调控的人单次跨膜蛋白质。他们通过生物信息学分析了人单次跨膜蛋白质的胞内区序列,发现它们的前10个氨基酸残基序列中富含带正电的碱性残基。由于细胞质膜的内层富含带负电的酸性磷脂,这些带正电的蛋白质很可能通过静电相互作用受酸性磷脂的调控,其中就包括CD28以及Nocth1、PD1L1、IL2RA等免疫系统中的关键功能蛋白。
据悉,该研究由许琛琦研究团队和牛津大学Omer Dushek研究团队合作完成,博士后杨魏(现任南方医科大学教授)、硕士生潘炜铃、陈硕凯、牛津大学博士生Trendel、博士生姜书谭为本文的共同第一作者,许琛琦研究员、李华副研究员和Omer Dushek教授为共同通讯作者。该项工作得到了上海交大沈红斌教授、上海科技大学王皞鹏教授、生物化学与细胞生物学研究所姜海、季红斌和刘小龙研究员的大力帮助,并得到国家自然科学基金委、中国科学院先导B专项以及科技部的经费支持。该研究工作还得到国家蛋白质科学设施(上海)核磁共振系统、显微成像系统,生化与细胞所细胞分析技术平台、分子生物学技术平台的大力支持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
39
#Biol#
37
#Bio#
25
#Struc#
28
#调控机制#
42
非常好的文章.学习了
62