妊娠期及哺乳期使用抗风湿病药物的全新英国推荐指南
2016-09-07 李常虹 刘湘源 中华风湿病学杂志
中华医学会神经病学分会 中华医学会神经病学分会脑血管病学组中华神经科杂志.2016,49(3):182-191颅内血管破裂后,血液流入蛛网膜下腔称为蛛网膜下腔出血(subarachnoid hemorrhage,SAH),临床上将SAH分为外伤性与非外伤性两大类。非外伤性SAH又称为自发性SAH,是一种常见且致死率极高的疾病,病因主要是动脉瘤,约占全部病例的85%左右,其他病因包括
中华医学会神经病学分会 中华医学会神经病学分会脑血管病学组
中华神经科杂志.2016,49(3):182-191
颅内血管破裂后,血液流入蛛网膜下腔称为蛛网膜下腔出血(subarachnoid hemorrhage,SAH),临床上将SAH分为外伤性与非外伤性两大类。非外伤性SAH又称为自发性SAH,是一种常见且致死率极高的疾病,病因主要是动脉瘤,约占全部病例的85%左右,其他病因包括中脑周围非动脉瘤性出血(perimesencephalic nonaneurysmal subarachnoid hemorrhage,PNSH)、血管畸形、硬脑膜动-静脉瘘(dural arteriovenous fistula,DAVF)、凝血功能障碍、吸食可卡因和垂体卒中等。近年来,血管介入技术、诊断方法与围手术期处理均有较大进展。但是,SAH患者的预后仍然较差,病死率高达45%,且存活者的残障率也较高。
中华医学会神经病学分会脑血管病学组2007年出版的《中国脑血管病防治指南》中包含有SAH的章节。中华医学会神经外科学分会曾于2006年出版枟临床疾病诊疗指南——神经外科》一书,其中也包含了SAH诊疗指南。近几年来不断有新的临床研究和相应的国际指南发表,几个多中心、前瞻性、随机对照试验和前瞻性队列研究对SAH的治疗提出了新的方法,因此,中华医学会神经病学分会及其脑血管病学组组织了对2007年版指南的重新修订,形成新版指南以指导临床医生的操作实践。由于其他原因的SAH的资料相对缺乏,故本指南主要是针对非外伤性、动脉瘤性SAH制定的。
危险因素及预防措施
危险因素
动脉瘤的危险因素分为3类:动脉瘤发生的危险因素,动脉瘤增大和形态改变的危险因素,动脉瘤破裂的危险因素。动脉瘤发生的危险因素包括不可调节和可调节两种。不可调节的因素包括高龄、女性、动脉瘤或SAH家族史和合并有相关疾病的高危人群。高危人群包括常染色体显性多囊肾病、IV型Ehlers-Danlos综合征、马凡综合征、主动脉狭窄、遗传性出血性毛细血管扩张症、肌纤维发育不良、动静脉畸形等。
多变量模型研究发现高血压、吸烟、酗酒均为SAH的独立危险因素。拟交感神经药包括可卡因和苯丙醇胺与SAH的发病相关。而这些SAH的危险因素恰巧也是多发性动脉瘤的危险因素(如吸烟、女性、高血压、脑血管病家族史及绝经期后)。
另外,天气和时间对于SAH的发病也有重要的影响。冬季和春季更易发病,也有研究发现气压与血压变化存在一定的联系,且与SAH的每天发病例数相关。
预防措施
目前尚无随机、对照试验提示哪种方法能降低SAH的发病率,观察性队列研究资料表明,对于年轻人来说,严格控制主要危险因素的效果较年老者好。尽管高血压是出血性卒中的危险因素之一,但缺乏控制血压对SAH发病率影响的研究资料。一项由117006名女性参加的前瞻性研究提示,戒烟可减少患SAH的风险,且戒烟时间与SAH风险呈负相关。
如果一级亲属中有2例以上动脉瘤性SAH者,建议做CT动脉造影(CTA)或MRA进行动脉瘤筛查。
推荐意见:
(1)SAH病死率很高,应该尽快行脑血管检查,以明确病因,及时治疗(I级推荐,B级证据)。(2)动脉瘤、高血压、吸烟、酗酒等为SAH的独立危险因素,滥用多种药物,如可卡因和苯丙醇胺与SAH的发病相关(I级推荐,B级证据)。(3)如果一级亲属中有2例以上动脉瘤性SAH者,建议做CTA或MRA进行动脉瘤筛查(III级推荐,C级证据)。
急诊诊断、评估和处理
一、SAH临床诊断和评估
大多数SAH患者因剧烈头痛急诊就医。头痛、脑膜刺激征阳性及头颅CT提示蛛网膜下腔呈高密度影是经典的诊断标准。SAH患者的急诊诊断和处理与患者的预后密切相关,且需要神经内、外科医生和放射科及神经血管医生共同合作完成早期的诊断,以免漏诊和误诊,贻误治疗。
(一)临床表现
患者常在体力劳动或激动时发病,主要表现为突然剧烈头痛,可伴恶心、呕吐、癫痫和脑膜刺激征,严重者可有意识障碍甚至很快死亡。少数表现不典型且头痛不严重的病例,容易导致延误诊断。
(二)影像学检查
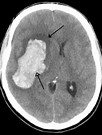
1.头颅CT平扫:CT是SAH诊断的首选。在SAH发病后12h内,CT的敏感度高达98%~100%,24h内逐渐降至93%,6d内降至57%~85%。CT可发现脑池和脑沟内的高密度影,有时脑室也有高密度出血影。但出血10d后或出血量较少时,CT检查可阴性。
2.CTA:CTA诊断动脉瘤的敏感度为77%~100%,特异度为79%~100%[12]。动脉瘤的大小、部位和影像设备质量影响着CTA检查的敏感度及特异度。当动脉瘤直径>5mm时,CTA的敏感度可达95%~100%,若动脉瘤直径<5mm,则敏感度仅为64%~83%。干扰CTA特异度的因素主要是血管管腔过于迂曲,可被误诊为颅内动脉瘤,多见于大脑中动脉分支区域、前交通动脉及小脑后下动脉。Velthuis等调查发现80%~83%的病例中CTA与DSA效果相同。经CTA检查后再行DSA检查,74%的患者结果相同。因此,凭CTA结果施行常规手术的做法是合理的,若因未行DSA而耽搁手术的做法缺乏依据。
CTA还可弥补DSA的不足,对于动脉瘤壁钙化、动脉瘤腔内血栓、动脉瘤导致脑实质出血的倾向及动脉瘤与骨性结构的关系等CTA具有一定优势。CTA具有快速成像、普及率广等优点,适用于急性重症患者。而CTA的缺点主要在于需使用碘造影剂、骨性伪影对成像质量产生干扰、对远端小血管尚不可及。CTA的伪影主要归咎于金属物质,因此动脉瘤已置入血管夹或弹簧圈的患者可能影响结果。随着CTA技术的不断完善,将更好地用于急性SAH的无创性诊断。
3.MRI和MRA:MRI也是确诊SAH的主要辅助诊断技术。FLAIR序列、质子密度成像、DWI、梯度回波序列有助于诊断。MRI在急性期的敏感度与CT相近,但随着病程的发展,其敏感度优于CT。因许多医院未开展急诊MRI检查、部分急症患者不配合检查、运动伪影、检查时间较长、费用高等问题限制其应用。
在SAH后的不同时间,MRI各序列的表现不同。发病数小时,T1WI为等或低信号,T2WI为等信号或高信号。发病24h后,出血处1iWI高信号、T2WI低或高信号、FLAIR、DWI均为高信号,而梯度回波或磁敏感加权成像(SWI)为低信号。
MRA尚不能在动脉瘤定位、定性方面替代DSA。三维时间飞跃法MRA诊断颅内动脉瘤的敏感度可达55%~93%。动脉瘤的大小决定了敏感度的高低,若动脉瘤直径>5mm,敏感度可达85%~100%;而若<5mm,则敏感度降至56%。MRA对于判断动脉瘤颈与所属血管的关系也存在着局限性。但MRA无需碘造影、无离子辐射,适用于孕妇,可用于SAH的病因筛查。
4.DSA:DSA是明确SAH病因、诊断颅内动脉瘤的“金标准”。首次DSA阴性的患者大约占20%~25%,1周后再行DSA,约有1%~2%患者发现之前未发现的动脉瘤。但是因为DSA有一定风险且费用偏高,是否一定行二次检查应因人而异。
(三)实验室和其他检查
若怀疑SAH,但急性期CT阴性,可行腰椎穿刺检查,如存在均匀血性脑脊液,可协助诊断少量的SAH。发病1周后,脑脊液黄变,显微镜下见大量皱缩红细胞,并可见吞噬了血红蛋白或含铁血黄素的巨噬细胞。
心电图检查有助于发现SAH引起的心肌受损,如P波高尖、QT间期延长和T波增高。血常规、血糖、出凝血功能、血气分析、心肌酶谱、心肌标志物、钩端螺旋体抗体等检查有助于判断病情及相关病因。
临床病程与体温和白细胞相关。入院时白细胞计数高于15x109/L或体温高于37.5℃,患者的病死率为55%~60%,上述两种情况发生血管痉挛的风险高,低于上述指标的患者,病死率为25%~35%。病程中可发生低钠血症,继发于抗利尿激素分泌不足,引起尿中的水和钠丢失,从而导致血容量减少和利尿性低钠血症。血小板计数、出血时间、凝血参数均应记录。血黏度增高伴血细胞比容超过40%,血清纤维蛋白原超过250mg,高渗透压等与预后不良有关。
(四)诊断和鉴别诊断
突发剧烈头痛,并伴有恶心、呕吐、意识障碍、癫痫、脑膜刺激征阳性及头颅CT检查发现蛛网膜下腔呈高密度影,即可确诊SAH。若头痛不严重,脑膜刺激征不明显,头颅CT检查未发现异常,但仍怀疑SAH,则尽早行腰椎穿刺检查,腰椎穿刺结果提示为均匀血性脑脊液,亦可确诊SAH。
SAH需要与脑膜炎、偏头痛发作鉴别。此外,有些颅内静脉窦血栓形成的患者,CT扫描有纵裂或横窦区域的高密度影,容易误判为SAH。
(五)病情评估和临床分级
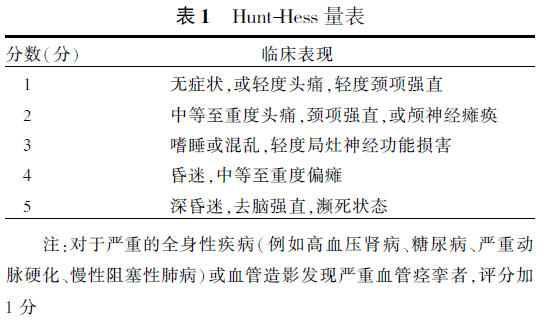
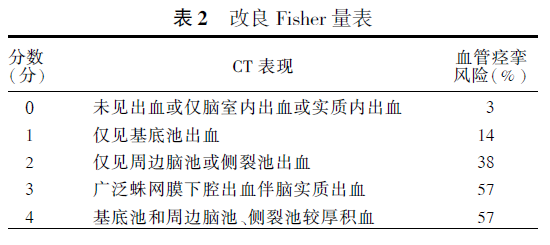
SAH患者的临床分级评分标准有多个版本,包括Hunt-HeSS量表(表1)、改良Fisher量表(主要评估血管痉挛的风险,表2)、格拉斯哥昏迷量表(GCS)等评分标准。尽管如何选择量表仍存争议,但仍推荐急诊时使用至少一种上述量表对患者进行评分并记录在案。
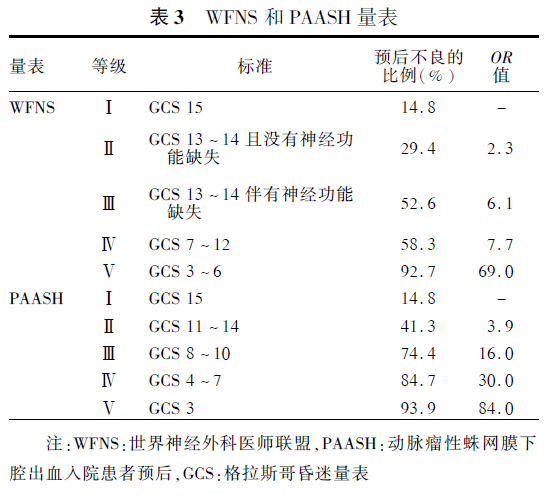
判断SAH患者预后常使用格拉斯哥预后评分,世界神经外科医师联盟(World Federation of Neurological Surgeons,WFNS)量表(表3)以及动脉瘤性SAH入院患者预后(Prognosison AdmissionofAneurysmal Subarachnoid Haemorrhage,PAASH;表3)量表评分。
患者就诊后应全面采集病史及完善相关体检,了解有无SAH危险因素、有无药物滥用史,年轻患者应予毒物筛查等。影响预后的相关因素如年龄、既往高血压史、就诊时间、入院时血压等均应记录在案。
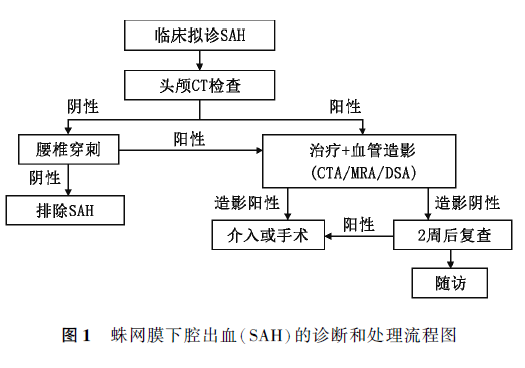
(六)SAH诊断和处理流程图SAH是神经科急症之一,需要迅速、正确的诊断和处理(图1)。
推荐意见:
(1)突发剧烈头痛伴脑膜刺激征阳性的患者应高度怀疑SAH诊断(I级推荐,B级证据)。(2)对可疑SAH患者应首选CT检查。(3)当CT结果阴性时,腰椎穿刺检查有助于进一步提供诊断信息(I级推荐,B级证据)。(4)对于SAH患者宜早期行DSA检查,以明确有无动脉瘤(I级推荐,B级证据)。(5)在DSA不能及时实施时,可予CTA或MRA检查(II级推荐,B级证据)。(6)动脉瘤介入治疗后,同时再做血管造影,以判断动脉瘤治疗的效果(I级推荐,B级证据)。(7)SAH评分有助于判断预后及采取不同的治疗手段。SAH早期应该使用GCS等工具进行评价(II级推荐,B级证据)。Hunt-Hess量表简单方便,临床常用于选择手术时的参考。在预后评估方面,PAASH量表比WFNS量表的效能更好。
二、SAH的监测和一般处理
SAH患者可能会出现各种并发症,如发热、血压和血糖升高,有意识障碍的患者还可能出现误吸及呼吸道阻塞等,其与预后相关,需要密切的监测和治疗。
(一)呼吸管理
保持呼吸道通畅,给予吸氧。虽然多数SAH患者不表现出气道受阻症状,但潜在的神经损伤可继发相关疾病,因此呼吸监护仍为第一要务。如果呼吸功能障碍,有必要气管插管,以维持气道通畅,保持正常血氧饱和度。
(二)血压管理
SAH并发高血压的管理应更为严格,应该及时使用效果较强的药物,静脉推注或持续滴注,控制血压。但血压过低容易诱发缺血性损伤。因此,血压控制的变异性大,不同病因、不同并发症状态下的处理不同。
至今尚无病例对照研究明确急性SAH患者控制血压对再出血的影响。一项综述分析发现服用降压药的患者其再出血风险降低,再出血可能与血压波动的关系较血压本身更密切。一项针对179例SAH患者的回顾性研究发现,在发病24h内入院的SAH患者中,17%的再出血患者收缩压曾达150mmHg(1mmHg=0.133kPa)。救护车上或初级医院中发病2h内的患者,再出血率为13.6%,且收缩压高于160mmHg的患者更易再出血。但有一项大型回顾性研究报道入院后再出血率为6.9%,且与血压无明显关联。由于这些研究观察时间不同,使用的抗高血压药物各异,结果存在差异。当血压偏高时,应予静脉持续给药,例如尼卡地平、拉贝洛尔及艾斯洛尔等。
(三)心电监护
国内学者回顾性研究800例SAH患者发现,发病3d内的患者66%出现心电图异常,主要表现为ST段抬高、水平下移或T波深度倒置。患者年龄、发病时意识障碍、Fisher分级以及合并脑疝、脑积水、脑血管痉挛等因素均与心电图异常相关,心电图异常与预后显著相关。因此建议对于急性SAH患者,应重视心电监护,采取积极的预防措施,保护心功能,改善患者的预后。
(四)水电解质平衡
据报道,SAH后发生低钠血症的概率约为10%~30%。低钠血症在前交通动脉瘤、脑积水等临床情况较差的病例中更为普遍。前瞻性、非对照研究提示低钠血症与过度的尿钠排泄和低血容量相关。延迟性缺血性神经功能缺损的发病率上升与体液减少相关,而且后者与脑血管痉挛也存在一定联系。2项随机对照研究证明了氟氢可的松可纠正低钠血症及体液平衡,因为激素能够纠正水钠负平衡,其次激素可减少对液体的需求并提高血钠浓度。另一项回顾性研究提出3%的氯化钠溶液可有效改善低钠血症,5%的白蛋白也有同样的作用。
(五)其他并发症
发热是SAH最常见的并发症,中枢性发热与病情的严重程度、出血量、血管痉挛的发展有关。发热是存活患者认知功能减退的独立预测因素。治疗发热能够改善患者的预后。但亚低温治疗却未能显示改善预后的治疗作用。
血糖的增高也是SAH患者预后不良的相关因素。控制血糖能改善预后。但是评分差的危重SAH患者,即使血糖正常,也存在脑内能量代谢危机和乳酸-丙酮酸比值的增高。一般建议空腹血糖控制在10mmol/L以下。
贫血也是SAH常见的一个并发症,前瞻性研究发现,高血红蛋白的患者预后较好。输注单采红细胞能提高SAH患者脑氧运输和脑氧利用率。但具体的血红蛋白水平尚未得知。
肝素诱发的血小板减少症发生率约为5%,但其发生与预防深静脉血栓时使用的肝素无关,而是与造影过程中使用的肝素量有关。发生肝素诱发的II型血小板减少症的患者更容易发生血栓类的并发症和症状性血管痉挛或迟发性脑缺血,病死率更高,预后更差。针对此并发症,似乎只能减少肝素的使用,改为使用其替代物。
深静脉血栓形成和肺栓塞是SAH尤其是有意识障碍的危重患者的常见并发症。可以使用弹力袜。高危患者可使用间断的充气压力装置进行预防。但是预防血栓需要使用低分子肝素的时间应控制在动脉瘤手术或栓塞12h以后。
严重头痛影响患者的情绪和睡眠,甚至促进血压升高。必要时可给予止痛剂治疗。
推荐意见:(1)注意保持呼吸道通畅(I级推荐,B级证据)。(2)注意监测血压,保持在收缩压<160mmHg和平均动脉压>90mmHg(I级推荐,C级证据)。(3)重视心电监护,采取积极的预防措施,保护心功能(II级推荐,B级证据)。(4)注意诊治低钠血症(I级推荐,B级证据)。(5)空腹血糖需控制在10mmol/L以下。(6)治疗发热,但是亚低温(33℃)治疗存在争议。
动脉瘤介入和外科手术治疗
推荐意见:
(1)外科手术夹闭或弹簧圈栓塞均可降低动脉瘤再破裂出血的风险(I级推荐,B级证据)。
(2)应尽可能选择完全栓塞治疗动脉瘤(I级推荐,B级证据)。
(3)动脉瘤的治疗方案应由经验丰富的神经外科与神经介入医师根据患者病情与动脉瘤情况共同商讨后决定(I级推荐,C级证据)。
(4)对于同时适用于介入栓塞及外科手术的动脉瘤患者,应首先考虑介入栓塞(I级推荐,A级证据)。
(5)支持手术夹闭的因素:年轻、合并血肿且有占位效应以及动脉瘤的因素(位置:大脑中动脉和胼胝体周围血管的动脉瘤;宽颈动脉瘤;动脉分支直接从动脉瘤囊发出);支持栓塞的因素:年龄超过70岁,无具有占位效应的血肿存在,动脉瘤因素(后循环、窄颈动脉瘤、单叶型动脉瘤),WFNS量表评分为IV级和V级的危重患者(II级推荐,C级证据)。
(6)早期治疗可降低再出血风险,球囊辅助栓塞、支架辅助栓塞和血流导向装置等新技术可提高早期动脉瘤治疗的有效性(II级推荐,B级证据)。
预防再出血的药物和其他治疗
推荐意见:
(1)针对病因治疗是预防再出血的根本措施(I级推荐,A级证据)。
(2)卧床休息有助于减少再出血,但需结合其他治疗措施(II级推荐,B级证据)。
(3)早期、短疗程抗纤溶药物如氨基己酸或氨甲环酸治疗可减少再出血的发生(II级推荐,B级证据)。
血管痉挛的监测和治疗
一、血管痉挛的判断和监测
推荐意见:
(1)血管痉挛在出血后的3~5d内开始出现,5~14d达到高峰,2~4周后逐渐缓解。
(2)新发的局灶性神经功能缺损,难以用脑积水或再出血解释时,应首先考虑为症状性血管痉挛。平均动脉压增高可能间接提示血管痉挛的发生。
(3)DSA判断血管痉挛的标准是:大脑中动脉主干或大脑前动脉A1段直径小于1mm,或大脑中动脉和大脑前动脉的远端支直径小于0.5mm(I级推荐,A级证据)。
(4)TCD判断标准为:TCD平均流速超过120cm/s或2次检查增加20cm/s与血管痉挛相关(n级推荐,B级证据)。
(5)推荐CT或MRI灌注成像明确脑缺血的范围(H级推荐,B级证据)。
二、血管痉挛的治疗
推荐意见:
(1)常规口服或静脉滴注尼莫地平,可有效防止动脉痉挛(I级推荐,A级证据)。
(2)维持有效的循环血容量可预防迟发性缺血(I级推荐,B级证据)。不推荐预防性应用高容量治疗和球囊扩张(III级推荐,B级证据)。
(3)动脉瘤治疗后,如发生动脉痉挛性脑缺血,可以诱导血压升高,但若血压已经很高或心脏情况不允许时则不能进行(I级推荐,B级证据)。
(4)如动脉痉挛对高血压治疗没有反应,可酌情选择脑血管成形术和(或)动脉内注射血管扩张剂治疗(III级推荐,B级证据)。
脑积水的治疗
急性脑积水(<72h内脑室扩张)发生率在15%~87%,临床评分或Fisher量表评分较差的病例更易出现急性脑积水。约1/3的急性脑积水患者没有症状,大约1/2的患者在24h内脑积水会自发缓解。但如果脑积水导致病情恶化或有脑疝风险,需要尽快行脑室外引流或者腰椎穿刺放液治疗,使颅内压维持在10~20mmHg。在脑室引流后,有40%~80%意识水平下降的患者有不同程度的改善。脑室引流与再出血的相关性尚未确定。
推荐意见:
(1)伴第三、四脑室积血的急性脑积水患者可考虑行脑室引流(I级推荐,B级证据)。(2)伴有症状的慢性脑积水患者可行临时或永久的脑脊液分流术(I级推荐,C级证据)。
癫痫样发作的治疗
已证实SAH后癫痫样发作与动脉瘤破裂有关,最近的回顾性研究报道癫痫样发作的发生率为6%~26%。大多数发作发生于就诊之前,在入院后予抗癫痫药物治疗后则几乎不发作,迟发性癫痫约占7%,回顾性研究发现其相关因素包括大脑中动脉动脉瘤、出血的厚度、伴发实质血肿、再出血、脑梗死、评分差以及有高血压病史。但目前尚缺乏癫痫样发作对预后影响的研究,所以不清楚其是否与预后不佳相关。
推荐意见:
(1)有明确癫痫发作的患者必须用药治疗,但是不主张预防性应用(II级推荐,B级证据)。(2)不推荐长期使用抗癫痫药物(III级推荐,B级证据)。但对既往有癫痫、脑出血、脑梗死、大脑中动脉动脉瘤破裂的癫痫样发作的高风险人群,可考虑长期使用抗癫痫药物(II级推荐,B级证据)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章,受益
52
继续学习
46
继续关注
40
继续学习
44
继续关注
49
学习学习。。。
25
#妊娠期#
29
#哺乳期#
28
#哺乳#
29
学习指南,更要应用指南。
22