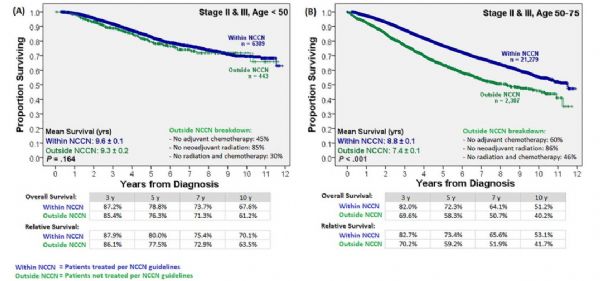
Cancer:4万人队列显示指南推荐的疗法对50岁以下直肠癌患者没有益处
2018-07-29 奇点糕 奇点网
结直肠癌在美国是发病第三高的癌症,在中国也是。大多数直肠癌患者都是50岁以上发病的,随着筛查的普及,这部分人群的直肠癌发病率也在逐年下降,但是50岁以下的年轻人中直肠癌发病却在上升。而且随着治疗措施的进步和筛查的普及,直肠癌的死亡率这些年下降了不少,但在50岁以下的年轻患者中死亡率却上升了。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












挑战指南了。
55
学习
0
学习
60
学习
54
好
53
阅
14