J Clin Med:肖格伦综合征与慢性鼻窦炎患者的相关性分析
2019-02-20 AlexYang MedSci原创
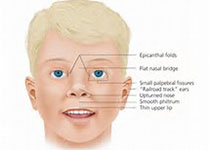
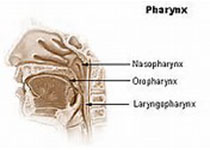
最近,有研究人员调查了慢性鼻窦炎(CRS)风险在肖格伦综合征(SS)患者中的情况。研究包括了18723名患有SS的患者,时间为1997年和2011之间。更多的是,59568名不患有SS的患者与患有SS的患者在性别、年龄、城市化水平、收入水平和鼻炎并发症以及鼻中隔偏曲匹配的比例为1:4。主要结果为CRS的发生率。研究发现,CRS在患有SS的患者中的累积发生率要比那些没有患SS的患者显著更高(p<
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#相关性#
27
#慢性鼻窦炎#
37
#综合征#
22
#相关性分析#
32
#肖格伦综合征#
22
#Med#
21