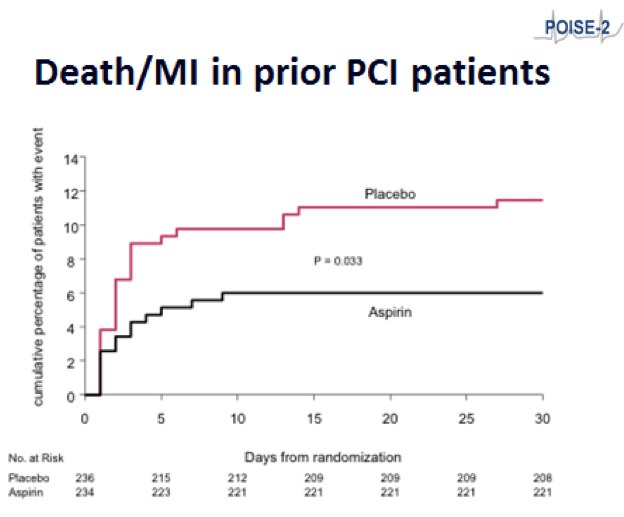
AHA2017:POISE-2研究:PCI后的非心脏手术,勿需停用阿司匹林
2017-11-19 天津医科大学总医院 董劭壮 杨清 壹生
在2017年AHA科学年会上,新近公布了POISE-2的PCI亚组分析的结果。研究者指出:对于既往有过PCI病史的患者,需要接受非心脏手术时,在围术期继续服用阿司匹林可能有益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非心脏#
33
#AHA#
30
#非心脏手术#
44
学习了新知识
71
谢谢分享学习了
74