Eur Respir J:COPD患者代谢组学分析确定了性别相关的代谢类型和氧化应激!
2017-07-09 xing.T MedSci原创
这些发现强调了氧化应激在COPD患者中的作用,提示性别增加了氧化应激失调,并可能通过自分泌运动因子-lysoPA轴,与疾病的机制和/或患病相关。
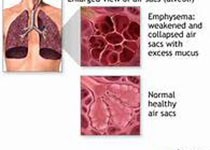
慢性阻塞性肺疾病(COPD)是一种异质性疾病,是世界范围内死亡和发病的主要原因。近日,呼吸疾病领域权威杂志Eur Respir J上发表了一篇研究文章,该研究旨在探讨COPD患者循环代谢谱的性别依赖性。
研究人员收集了斯卡COSMIC队列中健康不吸烟者(健康者)、肺功能正常的吸烟者(吸烟者)和COPD吸烟者(COPD;慢性阻塞性肺疾病全球倡议的阶段I-II/A-B)(n=116)的血清,并采用常规液相色谱-高分辨质谱的代谢组学平台进行分析。
通路分析表明多种改变的代谢产物参与氧化应激。有监督的多变量模型显示吸烟者根据COPD具有显著分类(P=2.8×10-7)。性别分层显示分离由女性所驱动(P=2.4×10-7),相比于男性(P=4×10-4)。使用靶向代谢组学定量证实显著改变的代谢产物。有针对性的代谢组学的多变量模型证实COPD女性患者代谢失调增加(P=3×10-3),相比于男性(P=0.10)。在COPD男性患者中,自分泌运动因子产生的lysoPA(16:0)和lysoPA(18:2)与肺功能(1 S用力呼气量)之间具有相关性(r=0.86;P<0.0001),但在女性患者中没有相关性(r=0.44;P=0.15),在肺脏中可以观察到与miR-29家族失调有关。
这些发现强调了氧化应激在COPD患者中的作用,提示性别增加了氧化应激失调,并可能通过自分泌运动因子-lysoPA轴,与疾病的机制和/或患病相关。
原始出处:
Shama Naz,et al. Metabolomics analysis identifies sex-associated metabotypes of oxidative stress and the autotaxin–lysoPA axis in COPD. Eur Respir J. http://erj.ersjournals.com/content/49/6/1602322
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









氧化应激在很多疾病的发病机制里有非常重要的角色
72
学习了.谢谢
59
#应激#
39
#代谢组#
43
#COPD患者#
24
学习一下
87
谢谢分享,学习了
75
学习了谢谢分享
0