Cancer cell:靶向组蛋白甲基酶PRMT1治疗急性髓系白血病
2016-01-21 佚名 生物谷
2016年1月20日讯 /生物谷BIOON/ --本文研究亮点: 通过AML融合转录因子招募PRMT1是白血病恶性转化所必需的过程但并非充分条件 MLL融合体以及MOZ-TIF2复合体能够招募去甲基化酶KDM4C移除H3K9me3这一抑制性甲基化标记 KDM4C和PRMT1负责调节AML疾病中异常的表观遗传和基因转录网络 通过分子或药物抑制KDM4C或者PRMT1能够抑制AML疾病发生
2016年1月20日讯 /生物谷BIOON/ --本文研究亮点:
通过AML融合转录因子招募PRMT1是白血病恶性转化所必需的过程但并非充分条件
MLL融合体以及MOZ-TIF2复合体能够招募去甲基化酶KDM4C移除H3K9me3这一抑制性甲基化标记
KDM4C和PRMT1负责调节AML疾病中异常的表观遗传和基因转录网络
通过分子或药物抑制KDM4C或者PRMT1能够抑制AML疾病发生

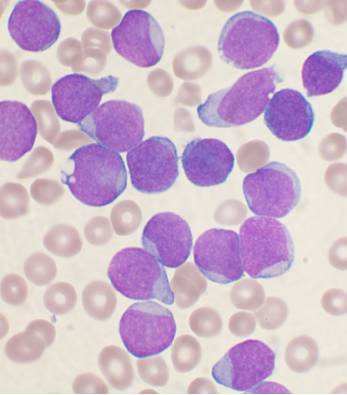
转录失调在急性髓系白血病的发病过程中具有重要作用,因此发现参与癌基因转录调控的表观遗传修饰酶可能是深入理解该疾病发病机制,开发有效治疗策略的关键所在。
近日,来自英国的科学家发现一种组蛋白甲基转移酶参与各种MLL以及非MLL白血病的发病过程,靶向该分子可能是治疗白血病的重要策略。
人类白血病的发病过程中经常存在染色体易位的情况,这会导致形成具有异常癌基因活性的嵌合体融合蛋白,开发一些小分子药物靶向这些融合蛋白已经成为一些白血病类型治疗的重要方法。但该方法在急性髓系白血病治疗方面的进展仍然很缓慢。
该研究发现的这种叫做PRMT1的酶是一种组蛋白精氨酸甲基转移酶,研究人员发现PRMT1是白血病恶性转化过程所必需的分子,但不足以诱导该过程的发生,白血病的恶性转化还需要通过嵌合转录因子招募另外一种分子——H3K9去甲基化酶KDM4C,共同介导表观遗传的重编程过程。利用药物抑制KDM4C/PRMT1能够进一步抑制MLL融合体以及MOZ-TIF2复合体促进癌基因转录和白血病恶性转化的能力。
这项研究阐述了组蛋白甲基化调控机制在白血病恶性转化过程中的作用,同时表明靶向表观遗传修饰酶可能是治疗白血病的一种有效策略,这项研究为白血病治疗提供了新的理论基础。
原始出处:
Ngai Cheung, Tsz Kan Fung,et al.Targeting Aberrant Epigenetic Networks Mediated by PRMT1 and KDM4C in Acute Myeloid Leukemia.Cancer Cell.Dec,2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#cancer cell#
24
#髓系白血病#
35
#Cell#
28
#CEL#
29
文章有深度
51
值得学习
142
#组蛋白#
24