BMJ:呼吸道没问题,但是持续性干咳,什么原因?
2016-09-28 MedSci MedSci原创
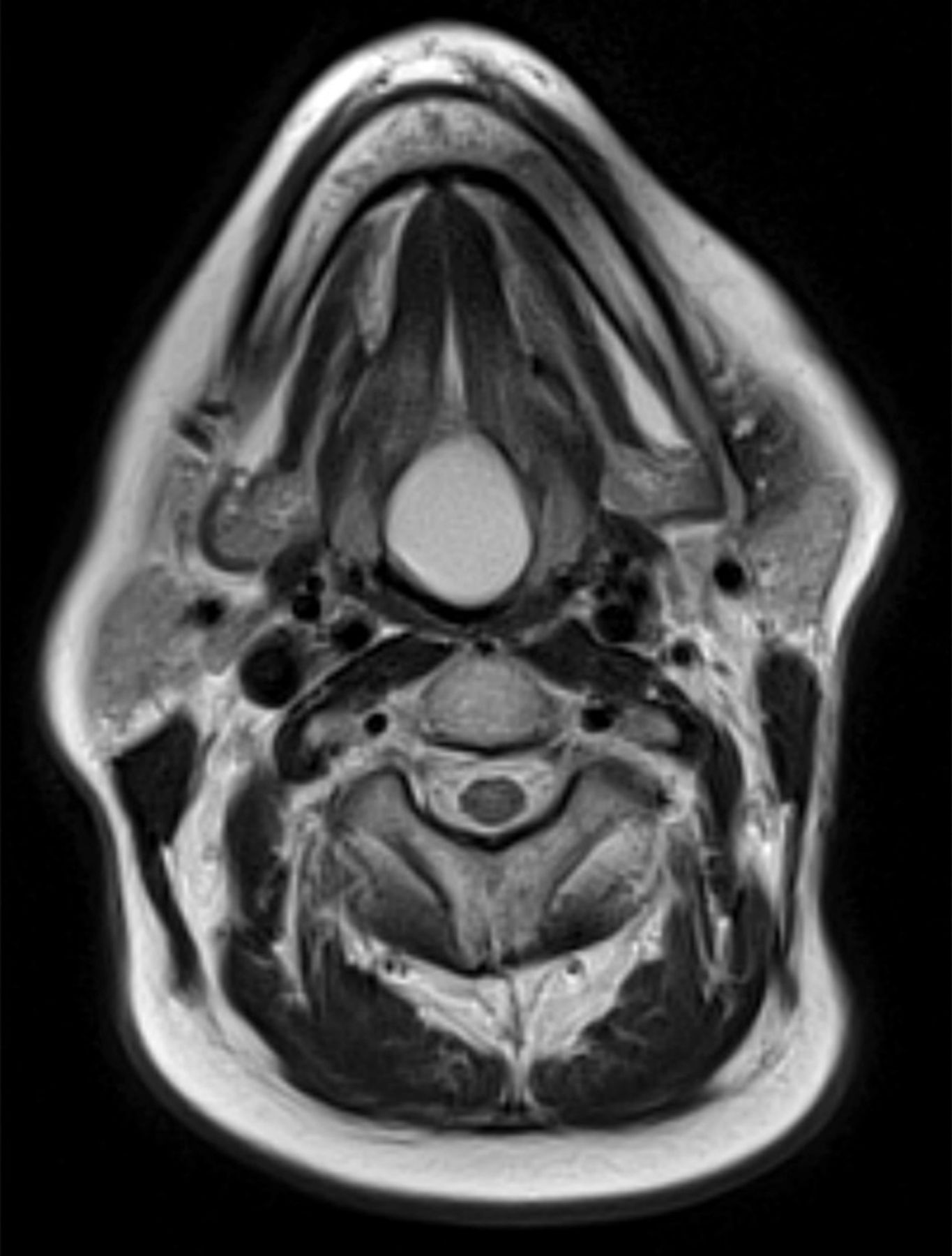
女性患者,60岁,因声音嘶哑和持续性的干咳而就诊。软性内窥镜显示患者舌后1/3有光滑、圆形肿胀物。该轴向T2加权磁共振图像显示舌根中线处有何异常(图1⇓)?诊断:残余的甲状舌管的囊性残余(甲状舌管囊肿)。磁共振图像显示在舌根后部有一个薄壁囊性病变,与甲状舌管囊肿(图2⇓)表现一致,在增强后T1加权矢状切面(图3⇓)也可看到。在头部和颈部中线处的囊性病变,鉴别诊断包括甲状舌管囊肿和皮样囊肿。图1显示
女性患者,60岁,因声音嘶哑和持续性的干咳而就诊。软性内窥镜显示患者舌后1/3有光滑、圆形肿胀物。
该轴向T2加权磁共振图像显示舌根中线处有何异常(图1⇓)?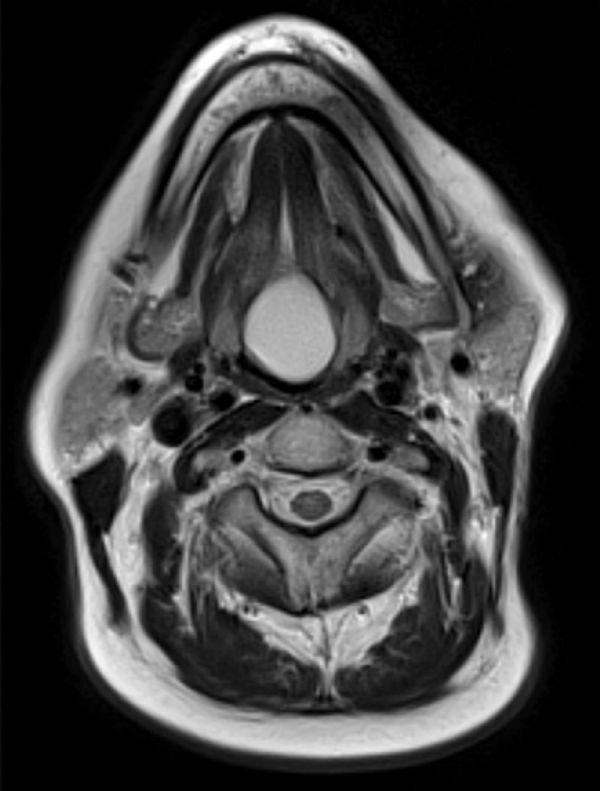
诊断:残余的甲状舌管的囊性结构(甲状舌管囊肿)。
磁共振图像显示在舌根后部有一个薄壁囊性病变,与甲状舌管囊肿(图2⇓)表现一致,在增强后T1加权矢状切面(图3⇓)也可看到。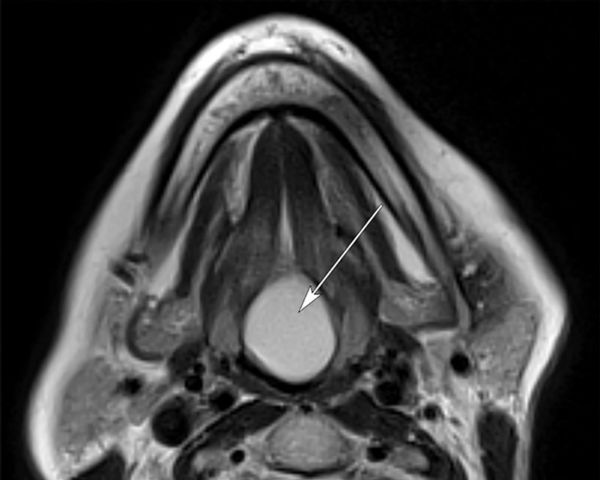

在头部和颈部中线处的囊性病变,鉴别诊断包括甲状舌管囊肿和皮样囊肿。图1显示甲状舌管囊肿样的表现,囊液均质。由于内含软组织和脂肪,皮样囊肿的异构现象较为明显。
甲状舌管囊肿是在头部和颈部最常见的先天性囊肿。常见于10岁及以下儿童,偶见于成人。甲状舌管是一种胚胎解剖结构,在甲状腺起始和终结的部位之间。若甲状腺下降至正常位置后,甲状舌管未能消失,仍作为连接舌后部和甲状腺的导管,那么将导致囊肿的形成。囊肿可形成于甲状舌管的任何地方,但最常用于舌骨和甲状软骨之间的部位。仅2%的囊肿发生于舌部位。
治疗方法最常用采用手术切除甲状舌管囊肿。手术的目的是通过切除囊肿、残余的甲状舌管和舌骨中段来降低复发率。由于囊肿易感染,且罕见情况子下可发生恶变,因此建议切除。
本病例中切除了患者的甲状舌管囊肿,且无并发症的发生。后其随访确认患者症状消失。
原始出处:
H L Adams, D C Howlett. A persistent cough. BMJ 2016; 354 doi: http://dx.doi.org/10.1136/bmj.i4858.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
21
#持续性#
39
#干咳#
30
好文章,受益
56
#呼吸道#
25