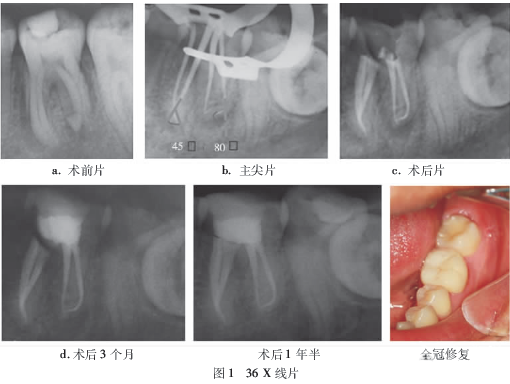
根管治疗过程牙周膜形成人造根管一例
2019-03-12 孙立众 王琳璇 王琦, 全科口腔医学电子杂志
患者,女,45岁,主诉因左上后牙不适1月来我院口腔科就诊。患牙不适1月,无自发性疼痛,无夜间疼痛,冷热刺激痛持续数分钟,咬合不适。无用药史,患牙未接受治疗。无药物过敏史。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#人造#
39
#牙周膜#
44
认真的学习努力学习好好学习
59
#牙周#
30
#根管#
27