神经鞘瘤误诊为颈动脉体瘤超声及CT表现1例
2018-12-19 杜鹏 曹爱红 中国CT和MRI杂志
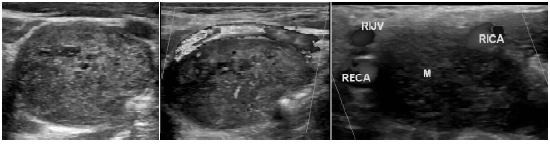
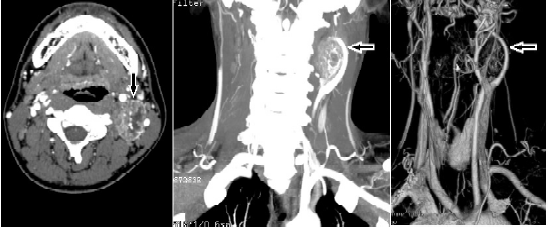
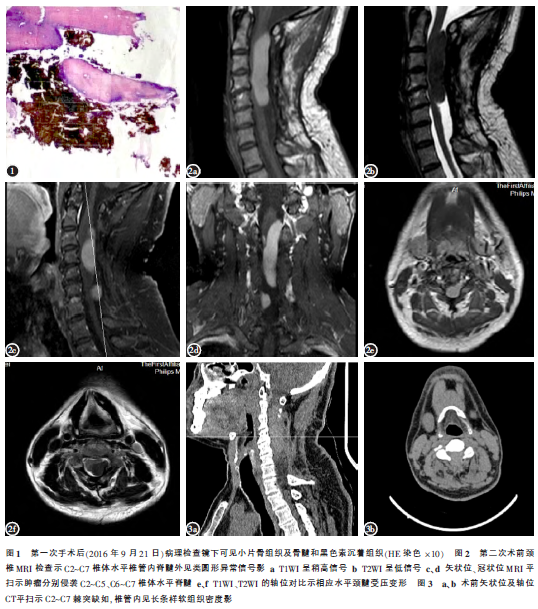
患者,男,20岁。因无意中发现左侧颈部肿物7d就诊,自觉无明显不适,专科查体:左侧颈部可触及一椭圆形肿物,呈搏动性,质中,境界清楚,活动度欠佳,不伴局部肿痛,不伴饮水呛咳和声音嘶哑,皮肤色泽正常,血压正常。行超声检查,左侧颈部皮下软组织内可见大小约4.1 cm×2.7 cm的低回声团,形态规则,边界清楚,位于颈内动脉与颈外动脉之间,CDFI:团块内可见条状血流信号,似可见颈动脉分支供血。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#颈动脉#
29
#神经鞘瘤#
47
#CT表现#
32
学习了
81