Circulation:巨噬细胞的Dicer通过调节线粒体氧化代谢抵制动脉粥样硬化
2018-11-03 MedSci MedSci原创
依赖线粒体氧化代谢的巨噬细胞激活在炎症和预防动脉粥样硬化中发挥核心作用。在动脉粥样硬化过程中,巨噬细胞需处理大量来自被吞噬的修饰的脂蛋白的胆固醇和甘油三酯。虽有多种microRNAs调控巨噬细胞极化,但在动脉粥样硬化过程中,microRNA生成酶Dicer在巨噬细胞激活中的作用尚不明确。为评估Dicer在动脉粥样硬化中的作用,研究人员采用高脂膳食饲养有/无特异性敲除巨噬细胞Dicer的Apoe-/
为评估Dicer在动脉粥样硬化中的作用,研究人员采用高脂膳食饲养有/无特异性敲除巨噬细胞Dicer的Apoe-/-小鼠12周。然后对小鼠进行抗-argonaute 2 RNA原位杂交和RNA深度测序,鉴定调节Dicer表型效应的microRNA和mRNA靶点。
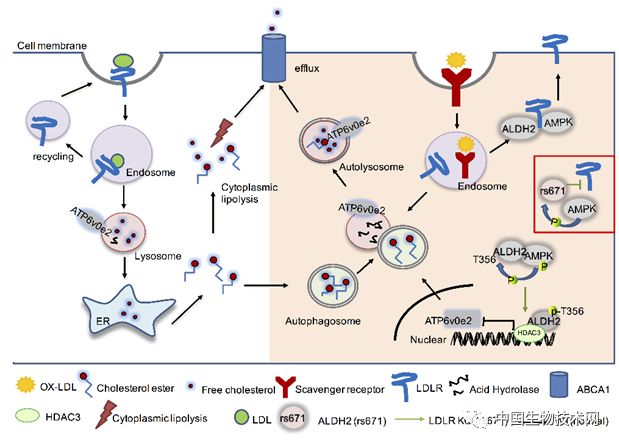
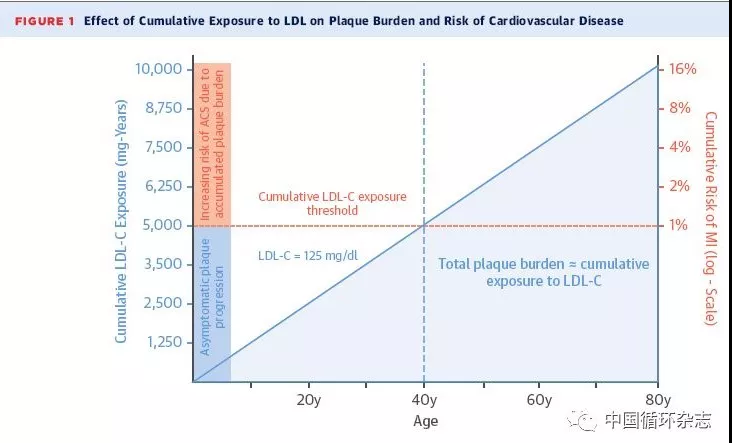
结果发现,敲除巨噬细胞的Dicer会加速小鼠的动脉粥样硬化,伴随炎症反应增强、病损处巨噬细胞内的脂质积累增多。在体外,由于线粒体脂肪酸氧化代谢受损,Dicer缺陷型巨噬细胞内的替代激活受限,充满脂质的泡沫细胞形成加快。恢复miR-10a、let-7b和miR-195a的表达可恢复激活改变的Dicer缺陷型巨噬细胞的氧化代谢。用miR-10a抑制配体依赖性核受体辅抑制因子,可促进脂肪酸氧化(介导Dicer的脂解和抗炎作用)。miR-10a的表达与人类动脉粥样硬化的进展呈负相关。采用靶位点阻滞剂封闭配体依赖性核受体辅抑制因子和miR-10a之间的相互作用可加剧小鼠的动脉粥样硬化进展。
Dicer通过增强以脂肪酸为燃料的线粒体呼吸,协调调节巨噬细胞的炎症反应和脂质代谢,从而发挥抗动脉粥样硬化的作用;提示促进巨噬细胞Dicer/miR-10a依赖性的代谢重编程或可应用于预防动脉粥样硬化。
Yuanyuan Wei,et al. Dicer in Macrophages Prevents Atherosclerosis by Promoting Mitochondrial Oxidative Metabolism. 24 Jul 2018. Circulation. 2018;138:2007–2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
35
#线粒体氧化代谢#
36
#ICER#
33
#DIC#
31