Cell:太"宅"的小鼠抵抗力差,移植肠道菌群可提高抗病力
2017-11-15 佚名 学术经纬
野生小鼠的肠道细菌的免疫学益处可能部分地解释了疾病研究中的持续性问题:为什么在实验室小鼠中进行的疾病实验,如疫苗研究,当转化到人类或其他动物中时结果变动非常大。
近日,顶尖学术期刊《细胞》上刊登了一项研究。科学家们发现,在接受野生小鼠的肠道细菌后,实验室小鼠的抗病能力有了显着提高!它们不但在感染致命流感病毒后得以存活,并且能更好地抗击结直肠癌。这项研究也让火热的微生物组领域持续升温。
野生小鼠的肠道细菌的免疫学益处可能部分地解释了疾病研究中的持续性问题:为什么在实验室小鼠中进行的疾病实验,如疫苗研究,当转化到人类或其他动物中时结果变动非常大。

▲本研究的主要负责人Barbara Rehermann博士(图片来源:NIH)
该文的资深作者,美国NIH糖尿病和消化和肾脏疾病研究所(NIDDK)肝脏疾病方向免疫科主任Barbara Rehermann博士说,“我们认为,通过恢复实验室小鼠的天然微生物身份,我们将能改进人类复杂疾病的建模”。
本文第一作者,NIDDK博士后研究员Stephan Rosshart博士说:“天然的微生物群落将有助于我们发现自然界相关的保护机制,而这在实验动物中是缺乏的。”
包括人类在内的哺乳动物的生活依赖于寄生在他们身上的微生物群落。进化塑造了每个动物的微生物群落,留下那些能够帮助动物在其环境和疾病中生存的微生物。但是实验室里的小鼠却与那些从地下室或田里随机抓的老鼠不同。
▲实验室小鼠有着稳定的遗传特性,却失去了野生小鼠的微生物菌落(图片来源:Pixabay)
实验室小鼠在严格控制的条件下繁殖和被喂养长大,这能保证每只小鼠具有可预测的性状和遗传学背景。这在基础生物学研究方面是一个很大的优势。但是,这也意味着人为创造出的受控环境而不是外界的生存压力,塑造了实验室小鼠的微生物群落。
Rosshart博士说:“实验室小鼠虽然对于了解基本的生物学而言至关重要,但是作为模型,其预测人体和其他哺乳动物复杂疾病反应的效果是有限的。
所以,研究人员试图让实验室老鼠得回自己失去的东西:自然共同进化的野生小鼠的肠道微生物菌群。研究人员从马里兰州和哥伦比亚特区的八个地点捕获了800多只野生小鼠,以寻找适合的健康肠道微生物菌群的供体。
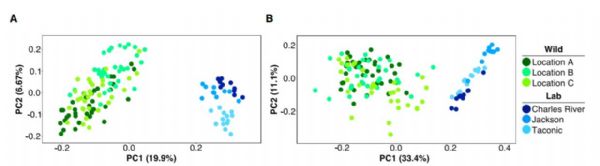
▲野生小鼠(绿色)和实验室小鼠(蓝色)的肠道菌群有显着不同(图片来源:《细胞》)
然后他们测试了多个来源的野生小鼠(Mus musculus domesticus)的肠微生物菌群基因组,并与实验室常用小鼠品系C57BL / 6对比。他们证实,C57BL / 6小鼠与野生小鼠具有不同的肠道微生物。
然后,研究人员将野生小鼠的微生物菌群移植入怀孕的无菌C57BL / 6小鼠中(WildR)。无菌小鼠在无菌环境中培养,没有自己的微生物。作为对照组,研究人员还将常规实验室C57BL / 6小鼠的微生物菌群移植到另一组怀孕的无菌C57BL / 6小鼠中(LabR)。四代后,这些小鼠仍携带从他们的前辈传下来的野生小鼠的微生物菌群或受控实验室小鼠品系的微生物菌群。
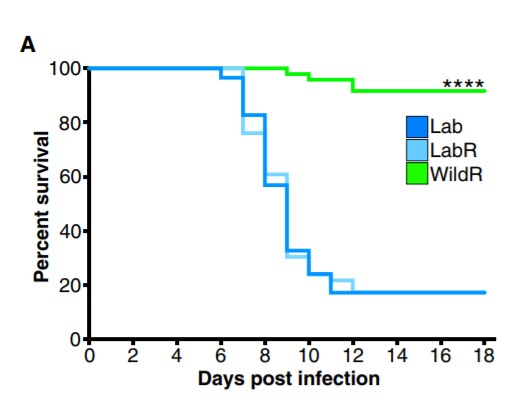
▲接受了高剂量的流感病毒后,只有野生小鼠菌群的小鼠(绿线)活了下来(图片来源:《细胞》)
当暴露于高剂量的流感病毒时,92%的具有野生微生物菌群的实验室小鼠存活了下来,而对照组中只有17%的实验室小鼠存活。在另一组实验中,具有野生微生物菌群的实验室小鼠在被诱导结肠直肠肿瘤后有更好的康复结果,而对照小鼠中则产生了更多的肿瘤和更严重的疾病。野生微生物菌群的有益作用与两种模型中的炎症减轻有关。
研究人员指出,需要更多的工作和评估来进一步确定结果,他们希望改进和扩展在实验室小鼠中使用天然微生物的方法。
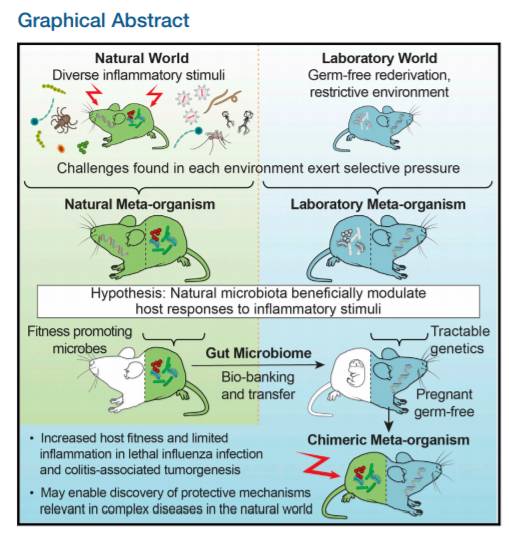
▲该研究的示意图(图片来源:《细胞》)
Rehermann博士说:“我们计划通过平行比较身体各部位的微生物菌群的各个组成部分,例如病毒和真菌等,来创建天然微生物菌群的完整微生物指纹图谱并研究其潜在的跨生物界相互作用。”
也许有一天,这项发现能带来更准确的疾病模型,或是带来提高免疫力的微生物疗法。
原始出处:Stephan P. Rosshart, Brian G. Vassallo, Davide Angeletti, et al. Wild Mouse Gut Microbiota Promotes Host Fitness and Improves Disease Resistance.Cell(2017)
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
36
#CEL#
41
学习了.获益匪浅!感谢分享
80
#肠道菌#
35
#抵抗力#
44
学习学习.了解了解
83