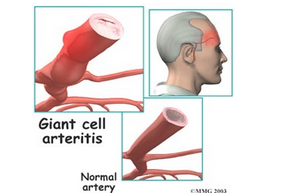
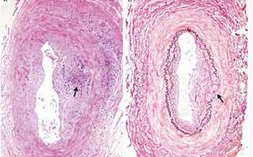
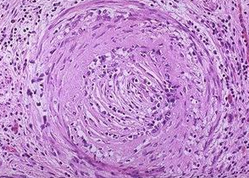
英国NHS同意罗氏的RoActemra(IL-6抗体)治疗巨细胞动脉炎
2018-04-20 MedSci MedSci原创
在英国NHS的成本监管机构的最后审批同意后,Roche的RoActemra将在未来三个月内为患有巨细胞动脉炎(GCA)的成年人定期提供。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉炎#
31
#EMR#
39
#英国NHS#
29
#IL-6#
33
#巨细胞#
31
#NHS#
36
#Actemra#
29
#RoActemra#
22
#MRA#
27
谢谢分享学习
52