Circulation.:AHA 右心衰竭的评估和管理科学声明:应用利尿剂重要
2018-04-24 佚名 中国循环杂志
近期,美国心脏协会(AHA)发布《右心衰竭的评估和管理科学声明》,对右心衰竭的病因、流行病学、病理生理学以及急慢性右心衰竭的管理进行了论述。
2 与左心室相比,右心室有不同的胚胎起源,在生理功能和解剖结构上存在不同,这解释了右心室对后负荷增加的敏感性。
3 右心衰竭常常与左心衰竭相关,有生存预测价值。
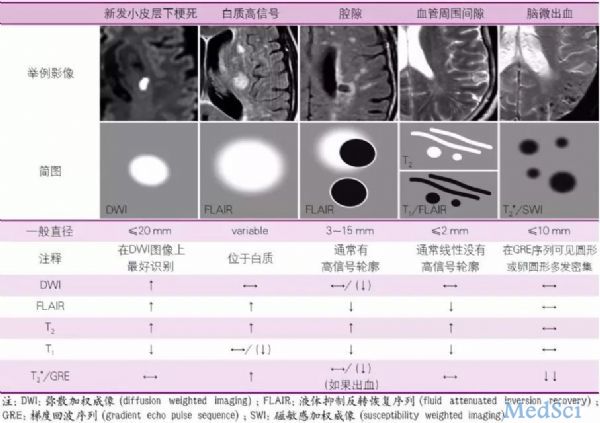
4 多种影像学成像模式用于评估右心室功能已经得到验证;然而,目前磁共振成像是测量体积、质量和收缩功能的金标准。
5 容量管理对急性右心衰竭的治疗至关重要,因为它会影响负荷情况、右心室功能、全身充血,但最重要的是心室相互依赖性,这会影响左心室充盈、每搏输出量和心输出量。
6 慢性右心衰竭管理的基石是口服利尿剂进行容量管理。其他治疗主要针对右心衰竭的病因,神经激素拮抗剂包括ACEI、β受体阻滞剂和盐皮质激素拮抗剂可能有益。
8 急性右心衰竭患者早期考虑机械循环支持很重要,这有助于右心室功能的恢复。
原始出处:
Konstam MA, Kiernan MS, Bernstein D, et al.Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association.Circulation. 2018 Apr 12. doi: 10.1161/CIR.0000000000000560. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#右心衰竭#
49
#右心衰#
44
#心衰竭#
41
#AHA#
32
#利尿剂#
26