苏格兰医药联盟积极推荐Darzalex作为多发性骨髓瘤的二线治疗方案
2019-07-09 Allan MedSci原创
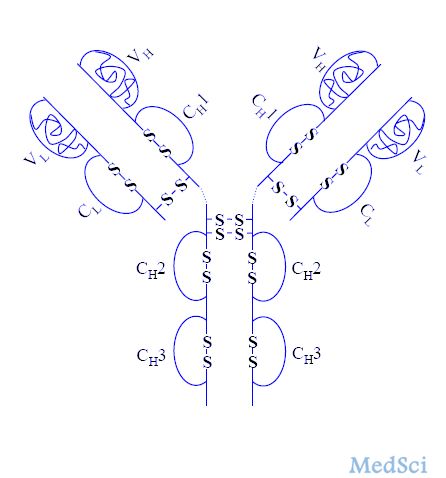
强生公司近日宣布,苏格兰医药联盟(SMC)积极推荐使用Darzalex®(daratumumab,达雷妥尤单抗)联合硼替佐米和地塞米松作为多发性骨髓瘤的二线治疗方案。
强生公司近日宣布,苏格兰医药联盟(SMC)积极推荐使用Darzalex®(daratumumab,达雷妥尤单抗)联合硼替佐米和地塞米松作为多发性骨髓瘤的二线治疗方案。
多发性骨髓瘤是由浆细胞引起的血癌。英国癌症研究中心的最新死亡率数据显示,2017年苏格兰有266例多发性骨髓瘤患者死亡。目前多发性骨髓瘤是无法治愈的,但治疗往往有助于控制症状和改善患者生活质量。使用标准疗法治疗后复发的患者预后较差,可用治疗方案很少。一项III期临床数据显示,接受达雷妥尤单抗、硼替佐米和地塞米松联合治疗的患者,其无进展生存期(PFS)显著延长。
原始出处:
http://www.firstwordpharma.com/node/1651923#axzz5syvQI0kQ
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
39
#治疗方案#
33
#苏格兰#
43
#医药#
26
#Darzalex#
36
#联盟#
28
#二线治疗#
31