ACS Appl. Mater. Interfaces:苏州医工所治疗肝癌的多功能纳米载药系统研究获进展
2018-01-30 佚名 苏州生物医学工程技术研究所
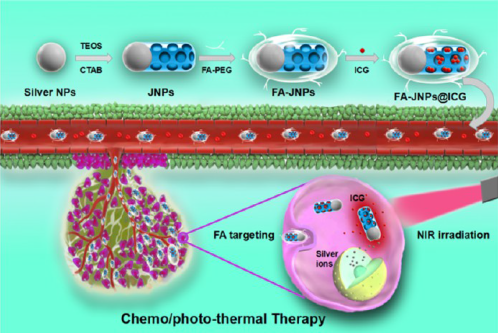
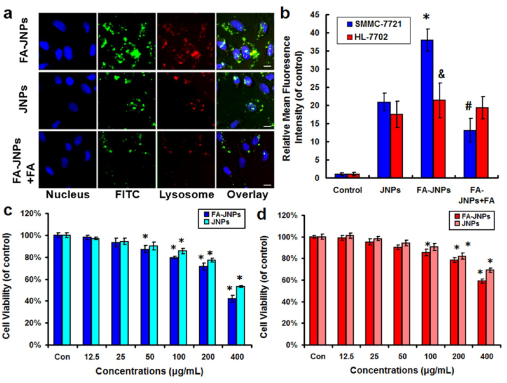
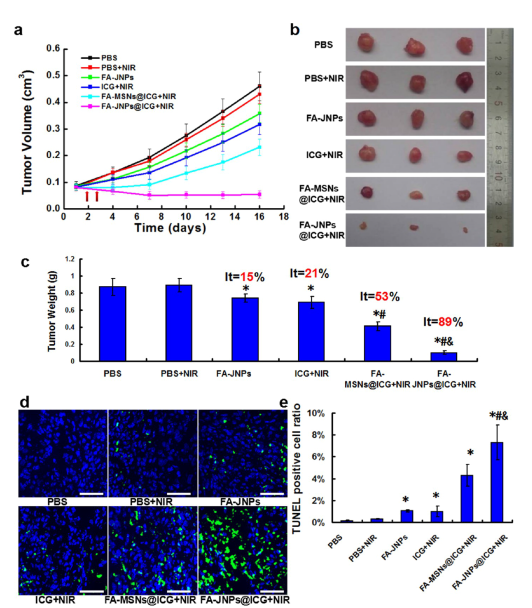
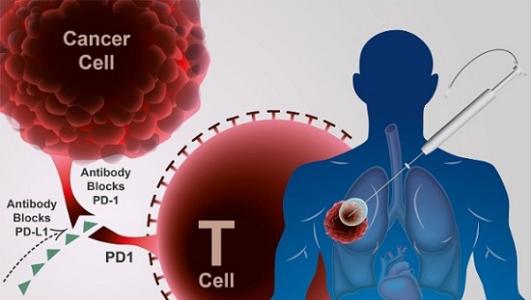
近些年来,科学家们发现了光热治疗的热效应可以促进银纳米材料释放银离子。而银离子在细胞内可以产生活性氧自由基,并通过线粒体凋亡途径诱导细胞凋亡。因此,银纳米材料协同光热治疗将是一种高效安全的肿瘤治疗策略。但相关研究面临难题和挑战,一是如何将光敏剂 ICG 和银纳米材料同时输送到肿瘤组织以增加癌症的治疗效果,二是如何开发一种开关去调控银离子的释放与 ICG 的剂量以增加治疗的安全性,三是如何提高其对肿
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#纳米载药#
37
#研究获进展#
34
#FAC#
34
#ACE#
36
#ACS#
44
不错的文章值得推荐
76
不错的文章.值得拥有
68