Circulation:动脉粥样硬化中的重要环节!
2017-02-02 MedSci MedSci原创
坏死的中心一直是脆弱的动脉粥样硬化斑块的标志。尽管凋亡细胞在几乎所有的其他组织床中可以被迅速清除,但是在病变血管中它们的去除似乎显着受损。最新的证据表明,这种现象是由胞葬作用(Efferocytosis)缺陷引起的,一种凋亡组织被吞噬细胞(如巨噬细胞)识别并吞噬的过程。遗传和实验数据表明,胞葬作用受损发生在动脉粥样硬化造成的所谓的“吃我配体”失调中,它可以调控决经历程序性细胞死亡的细胞吞噬。以下是
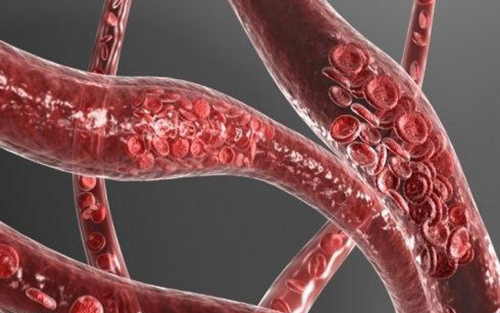
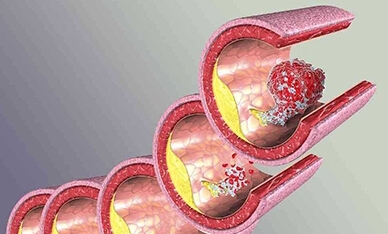
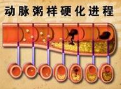
坏死的中心一直是脆弱的动脉粥样硬化斑块的标志。尽管凋亡细胞在几乎所有的其他组织床中可以被迅速清除,但是在病变血管中它们的去除似乎显着受损。
最新的证据表明,这种现象是由胞葬作用(Efferocytosis)缺陷引起的,一种凋亡组织被吞噬细胞(如巨噬细胞)识别并吞噬的过程。
遗传和实验数据表明,胞葬作用受损发生在动脉粥样硬化造成的所谓的“吃我配体”失调中,它可以调控决经历程序性细胞死亡的细胞吞噬。
以下是最近数据的总结,其指示胞葬作用是损伤扩大的主要不受欢迎的驱动因素,但是也可能作为防止斑块进展的潜在靶点的可逆性缺陷。
原始出处:
Kojima Y, Weissman IL, Leeper NJ. The Role of Efferocytosis in Atherosclerosis. Circulation. 2017 Jan 31;135(5):476-489.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重要环节#
41
#粥样硬化#
28
很受益
48
学习。。。。。
58
嗯,学习了新的内容
79
长见识了
56
稳定斑块,避免斑块脱落
70