斜坡孤立性浆细胞瘤1例
2019-07-29 吴佳栗 范国光 医学影像学杂志
患者男,61岁。以“视物重影伴头疼10天”入院。糖尿病史多年,血糖控制可。患者无明显诱因出现视物重影10天,自述右眼感觉异常,视物成双,头疼胀痛,休息后无缓解;于外院行MRI提示岩斜区肿物,未行治疗。
患者男,61岁。以“视物重影伴头疼10天”入院。糖尿病史多年,血糖控制可。患者无明显诱因出现视物重影10天,自述右眼感觉异常,视物成双,头疼胀痛,休息后无缓解;于外院行MRI提示岩斜区肿物,未行治疗。
颅脑CT+颅脑MR平扫、增强。CT表现提示鞍区偏右侧可见团块状密度增高影,病灶向右前方突入蝶窦,蝶窦后壁及斜坡、右侧岩尖骨质被破坏吸收;鞍区MRI平扫+增强提示斜坡可见等信号团块影,大小约为3 cm×4 cm,增强扫描肿块不均匀强化(图1~6)。诊断:颅底中线区占位性病变,临床拟诊为脊索瘤。
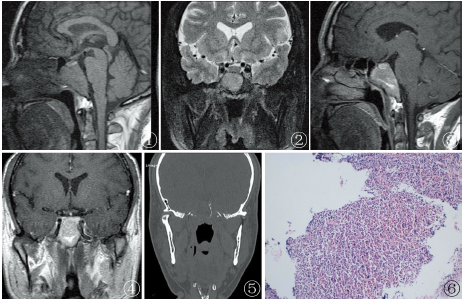
图1,2斜坡肿块T1WI及T2WI呈等信号;图3,4增强扫描呈条片状不均匀强化;图5右侧岩尖骨质被破坏吸收;图6组织内见异型浆细胞弥漫增生,巢状排列且密集
手术及病理:切除后送病理镜下所见:组织内见异型浆细胞弥漫增生,巢状排列,排列密集。免疫组化:ACTH(+)Ki-67(约30%+)MUM1(+)CD79a(+)CD138(+)。病理诊断:(斜坡肿块)免疫组化结果支持为浆细胞瘤。
讨论:
浆细胞瘤是起源于骨髓造血组织的一种原发的全身性肿瘤。孤立性浆细胞瘤多发生于全身,鲜少发生在颅底。颅底浆细胞瘤一旦发生,易发生在眼眶,蝶窦和鞍背。本例发生在斜坡,文献报道以个案报道为主,好发于50~60岁女性,常见症状为头痛、脑神经受压导致的视觉功能障碍及内分泌失调。斜坡孤立性浆细胞瘤在大体上质软脆,缓慢深入组织生长,对骨组织造成破坏,组织学上组成较单一,由不同程度的异型性浆细胞构成,无明显伴淋巴细胞浸润。故CT表现为均匀稍高密度影,病灶处骨质发生穿凿样溶骨性、膨胀性、虫噬样骨质破坏,骨皮质不完整,骨破坏区边缘可见环形壳状残存骨质结构,缺乏骨硬化和骨膜反应,MRI呈等或稍长T1信号,等或稍短T2信号,肿瘤内增强扫描后均匀强化。
斜坡区最好发脊索瘤,质软、呈胶冻样多小叶状肿块并有假包膜。另外,瘤组织中可残留碎骨性或骨小梁间隔,软组织钙化,易出血、坏死和囊变,因此脊索瘤CT表现特点为肿块内不规则斑片状钙化影,MRI中T1WI呈低-中等信号伴点状高信号,增强扫描呈不均匀强化;由于脊索瘤由大的空泡状的粘液细胞组成,T2WI呈极高信号。因此,二者由于组织成分的不同,在影像学上存在一定的差异,斜坡孤立性浆细胞瘤以等信号为主,并且增强扫描均匀强化,而脊索瘤在T1WI呈低-中等信号伴点状高信号,T2WI呈极高信号,增强扫描强化不均;本病例T1、T2信号变化与文献报道接近,但增强扫描呈条片状不均匀强化,提示强化信号变异可能较大,与肿瘤血运有关,需要注意并与脊索瘤鉴别。此外,斜坡孤立性浆细胞瘤影像学上还应与颅底肉瘤、垂体腺瘤、脑膜瘤和转移性肿瘤相鉴别。
原始出处:
吴佳栗,范国光.斜坡孤立性浆细胞瘤1例[J].医学影像学杂志,2018(04):537+541.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#浆细胞瘤#
34
#浆细胞#
35
#细胞瘤#
25
#孤立性#
37