JAMA子刊:钝性或穿透性创伤后的静脉血栓栓塞风险研究
2016-10-12 MedSci MedSci原创
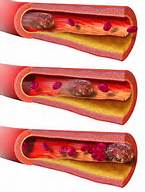
到目前为止,没有研究评估钝性或穿透性创伤后,静脉血栓栓塞(VTE)风险是否会发生变化。研究纳入813例闭合性创伤患者(平均[SD]年龄,47 [ 19 ]岁)和324例穿透伤创伤患者(平均[SD]年龄,35 [ 15 ]岁),总体VTE发生率为9.1%(104/1137),两组间VTE发生率相似(钝伤,9% [n = 73] vs 穿透伤,9.6% [n = 31]; P = .76)。钝伤组中,
到目前为止,没有研究评估钝性或穿透性创伤后,静脉血栓栓塞(VTE)风险是否会发生变化。
研究纳入813例闭合性创伤患者(平均[SD]年龄,47 [ 19 ]岁)和324例穿透伤创伤患者(平均[SD]年龄,35 [ 15 ]岁),总体VTE发生率为9.1%(104/1137),两组间VTE发生率相似(钝伤,9% [n = 73] vs 穿透伤,9.6% [n = 31]; P = .76)。
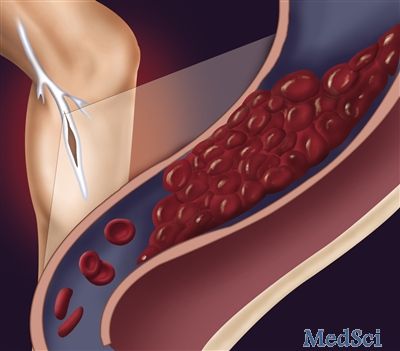
钝伤组中,VTE患者与非VTE患者比较,有凝血异常的患者更多(49.3% vs 35.7%; P = .02)、股动脉导管的患者更多(9.6% vs 3.9%; P = .03)、修复和/或结扎血管损伤的患者更多(15.1% vs 5.4%; P = .001)、复杂的腿骨折患者更多(34.2% vs 18.5%; P = .001)、格拉斯哥昏迷量表评分小于8的患者更多(31.5% vs 10.7%; P < .001)、4或更多次输血的患者更多(51.4% vs 17.6%; P < .001)、手术时间超过2小时的患者更多(35.6% vs 16.4%; P < .001)、骨盆骨折患者更多(43.8% vs 21.4%; P < .001)、VTE患者也有更高的平均(SD)格林菲尔德风险评估量表评分 (13 [6] vs 8 [4]; P ≤ .001)。
然而,在多变量分析中,只有接收4个或更多的输血(OR, 3.47; 95% CI, 2.04-5.91)、格拉斯哥昏迷量表评分小于8(OR, 2.75; 95% CI, 1.53-4.94)、骨盆骨折(OR, 2.09; 95% CI, 1.23-3.55)可以预测VTE,ROC曲线下面积为0.730。
在穿透性创伤组,VTE患者与非VTE患者比较,以下情况的患者比例更多:凝血结果异常(64.5% vs 44.4%; P = .03)、股动脉导管(16.1% vs 5.5%; P = .02)、修复和/或结扎血管损伤(54.8% vs 25.3%; P < .001)、4或更多次输血(74.2% vs 39.6%; P < .001)、手术时间超过2小时(74.2% vs 50.5%; P = .01)、简短腹部损伤评分大于2(64.5% vs 42.3%; P = .02)、40到59年(41.9% vs 23.2%; P = .02)、VTE患者也有更高的平均(SD)格林菲尔德风险评估量表评分(12 [4] vs 7 [4]; P < .001)。
然而,在多变量分析中,只有修复和/或结扎血管损伤(OR, 3.32; 95% CI, 1.37-8.03)、简短腹部损伤评分大于2(OR, 2.77; 95% CI, 1.19-6.45)和40岁到59岁(OR, 2.69; 95% CI, 1.19-6.08)可以预测VTE,ROC曲线下面积为0.760。
虽然钝性和穿透性创伤患者的VTE发生率是相同的,但是基于损伤机制不同,两组患者的VTE独立危险因素是有差异的。基于这一项发现,应分别考虑不同的预防性治疗方案。
原始出处:
Charles A. Karcutskie, MD, MA1,2; Jonathan P. Meizoso, MD1,2; Juliet J. Ray, MD1,2; et al.Association of Mechanism of Injury With Risk for Venous Thromboembolism After Trauma. JAMA Surg. Published online September 28, 2016. doi:10.1001/jamasurg.2016.3116
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险研究#
32
#静脉血栓栓塞风险#
41
#静脉#
30
#静脉血#
24
谢谢学习
46
#创伤#
19
这个挺有意思的
41