盘点:近期关于丙肝药-索非布韦的研究进展一览
2017-10-05 lishiting MedSci原创
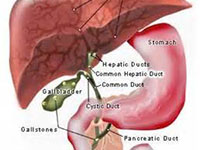
近日,重磅丙肝药索非布韦已通过审批,意味着它即将进入中国市场开疆拓土。索非布韦为美国吉利德公司开发的治疗慢性丙肝新药。有报道显示,该药是首个无需联合干扰素就能安全有效的治疗某些类型的丙肝。在此,小编整理了近期对索非布韦的研究进展一览。【1】Eur J Gastroenterol Hepatol:Sofosbuvir、daclatasvir联合利巴韦林治疗改善慢性丙型肝炎患者肝功能直接抗病毒药物
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#丙肝药#
41
学习了.非常好的资讯.谢谢
43
#研究进展#
22
#索非布韦#
32
henhao
43
学习了.谢谢.这类药物可以研究.
48
学习一下谢谢分享
45
文章很好.值得分享
46
学习
20
学习谢谢分享
15