JCO:CD33剪接多态性决定AML患者对吉妥单抗的响应(III期临床研究)
2017-06-26 xiaoxiao MedSci原创
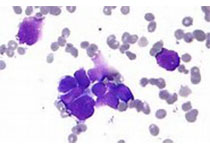
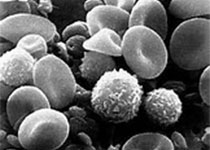
吉妥单抗(Gemtuzumab ozogamicin,GO)来源于重组人源化抗CD33单抗与细胞毒药物卡奇霉素的复合物,是一种靶向CD33的免疫偶联物,常被用于治疗治疗急性髓系白血病(AML)。其作用机制为:CD33表达于80%以上的急性髓性白血病(AML)患者白血病细胞上。本品静脉注射后,偶联屋中的抗体与复合物可被靶细胞胞饮。在细胞内,卡奇霉素从偶联物上水解游离,与DNA结合,使其双螺旋断列,导
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#I期临床#
29
#JCO#
24
#III#
34
#II期临床研究#
27
#III期临床研究#
24
#吉妥单抗#
32
#II期临床#
22
#CD33#
0
#III期#
18
#多态性#
35