Nat Med:中国学者揭密骨质疏松和骨肿瘤关键信号通路
2016-04-22 刘明耀等 《自然—医学》
4月12日,《自然—医学》在线发表了华东师大刘明耀、罗剑课题组和第二军医大学附属上海长征医院肖建如课题组关于骨质疏松和骨肿瘤治疗的最新发现,该成果的药物开发具有很高的应用价值。据介绍,患有骨质疏松症和骨肿瘤的人群日益增多,但临床上对这些疾病的认识和治疗还存在较大不足。在这项研究中,课题组联合攻关,在原有多项成果基础上展开深入研究,发现LGR4是破骨细胞中最重要细胞分化因子RANKL的新受体,进而深
4月12日,《自然—医学》在线发表了华东师大刘明耀、罗剑课题组和第二军医大学附属上海长征医院肖建如课题组关于骨质疏松和骨肿瘤治疗的最新发现,该成果的药物开发具有很高的应用价值。
据介绍,患有骨质疏松症和骨肿瘤的人群日益增多,但临床上对这些疾病的认识和治疗还存在较大不足。
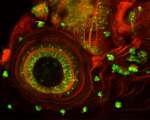
在这项研究中,课题组联合攻关,在原有多项成果基础上展开深入研究,发现LGR4是破骨细胞中最重要细胞分化因子RANKL的新受体,进而深入挖掘其分子机理,并基于此开发了以LGR4为靶标的蛋白抑制剂。实验表明,该蛋白抑制剂能显著抑制骨质疏松和骨肿瘤等骨科疾病,而相关药物学研究也证明了RANKL/LGR4信号通路在这些疾病中的关键作用。
这项研究工作受到国际审稿专家的高度评价。同时,该成果已申请国家发明专利。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
0
不错啊!
77
学习了,很好的
100
#信号通路#
26
#骨质#
28
#Med#
19
骨质疏松,好好防治
87
很好!
92
文章不错哦
96
不错的思路
76