AHA 2016:旁观者CRP能提高院外心脏骤停患儿的生存率
2016-11-13 MedSci MedSci原创
据美国心脏协会科学会议上发表的一项研究结果显示,对于院外心脏骤停儿童患者,旁观者心肺复苏术能获得生存益处;常规的旁观者心肺复苏与仅按压的旁观者心肺复苏相比,患者能得到更好的结局。 研究人员分析了3900例年龄小于18岁的非创伤性院外心脏骤停患者的数据,其中,婴幼儿占59.4%,女性占60.2%,不可电击复律心律占92.2%。 主要感兴趣的结局是总生存率和神经功能良好的生存率,定义为出院
据美国心脏协会科学会议上发表的一项研究结果显示,对于院外心脏骤停儿童患者,旁观者心肺复苏术能获得生存益处;常规的旁观者心肺复苏与仅按压的旁观者心肺复苏相比,患者能得到更好的结局。
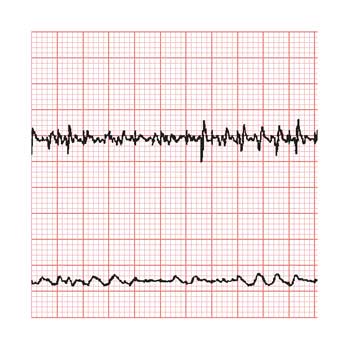
研究人员分析了3900例年龄小于18岁的非创伤性院外心脏骤停患者的数据,其中,婴幼儿占59.4%,女性占60.2%,不可电击复律心律占92.2%。
主要感兴趣的结局是总生存率和神经功能良好的生存率,定义为出院时脑性能类别评分1或2。根据种族、是否有旁观者心肺复苏和旁观者心肺复苏类型(常规或仅按压)对患者进行分层。
来自宾夕法尼亚大学费城儿童医院心脏中心的研究者Maryam Y. Naim博士称:“队列中46.5%的患儿进行了旁观者CPR,白人(56.3%)患儿进行旁观者CPR的比例大于黑人(39.4%)和西班牙裔儿童(43.3%; P < .001)。”
在整个队列中,总生存率为11.3%,神经功能良好的生存率为9.1%。
当Naim与同事进行多变量分析后发现,旁观者CPR与更好的生存相关(调整后的比例,13.2%; 95% CI, 11.81-14.58;aOR = 1.57; 95% CI, 1.25-1.96),与更好的神经功能良好的生存率(调整后的比例, 10.3%; 95% CI, 9.1-11.54; aOR = 1.5; 95% CI, 1.21-1.98)。
对于那些没有接受旁观者CPR的患儿,调整后的总体生存率为9.5%(95% CI, 8.28-10.69),调整后的神经功能良好的生存率为7.59%; 95% CI, 6.5-8.68)。
对于接受旁观者CPR的患儿,接受常规CPR和仅按压的CPR的比例分别为49.4%和50.6%。
多变量分析结果显示,常规CPR与没有接受CRP的患者相比,与神经功能良好的生存率有关(常规CPR:调整后的比例,12.89%; 95% CI, 10.69-15.09;没有CRP:调整后的比例,9.59; 95% CI, 6.45-8.61;aOR = 2.06; 95% CI, 1.51-2.79)。
对于婴儿,常规CPR与没有接受CRP的患者相比,有更高的生存率结局,但是并没有发现仅按压的CPR与更好的生存率之间的联系。
对于1岁至18岁的儿童,两种类型的CRP与没有接受CRP的患者相比,均与更好的结局有关。
原始出处:
Naim MY, et al. Presentation 20. Presented at: American Heart Association Scientific Sessions; Nov. 12-16, 2016; New Orleans.
Conventional bystander CPR benefits children with out-of-hospital cardiac arrest.Healio.November 12, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#生存率#
25
#AHA#
25
#CRP#
21
#院外心脏骤停#
24
学习的
60