Cancer Discov:这项新发现有望减少CAR-T疗法副作用
2017-10-16 佚名 药明康德
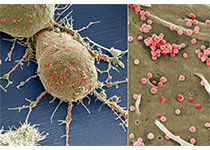
尽管癌症研究者们因最近诺华CAR-T疗法Kymriah获得FDA批准而感到兴奋,但是对于其副作用的担忧依然困扰着学界。在诺华的这一疗法以及其它类似疗法的临床试验中,一些患者发生了称为细胞因子释放综合征的危险的免疫反应,还有一部分患者发生神经毒性。这些副作用严重时可能危及生命。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新发现#
21
#Dis#
26
#副作用#
30
#CAR-#
30
学习了谢谢分享!!
59
#ISC#
30