Blood:伊布替尼单药治疗慢性淋巴细胞白血病5年随访结果公布!
2018-05-09 Alicia 肿瘤资讯
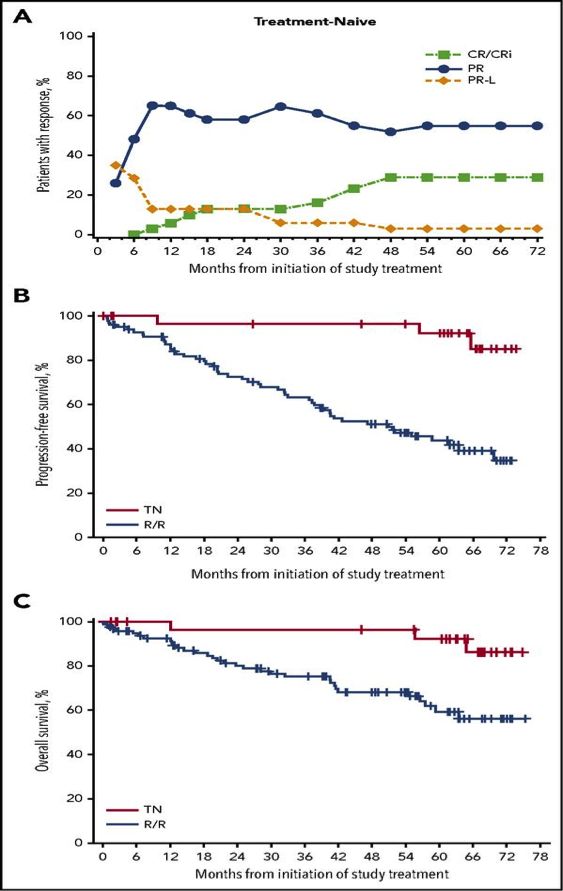
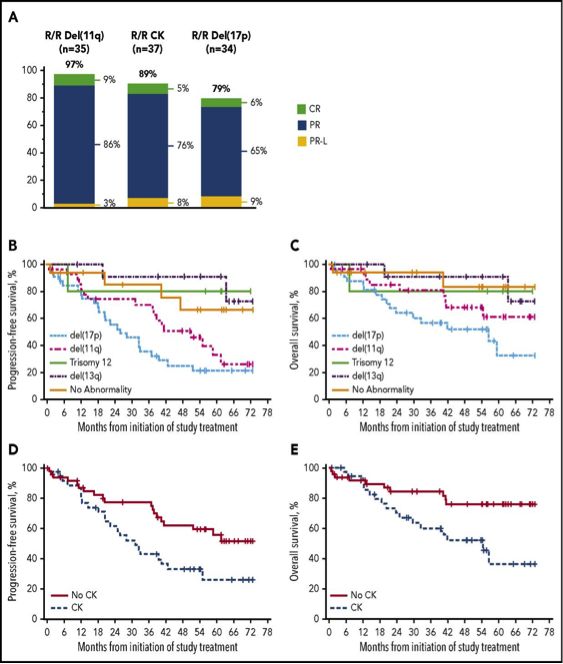
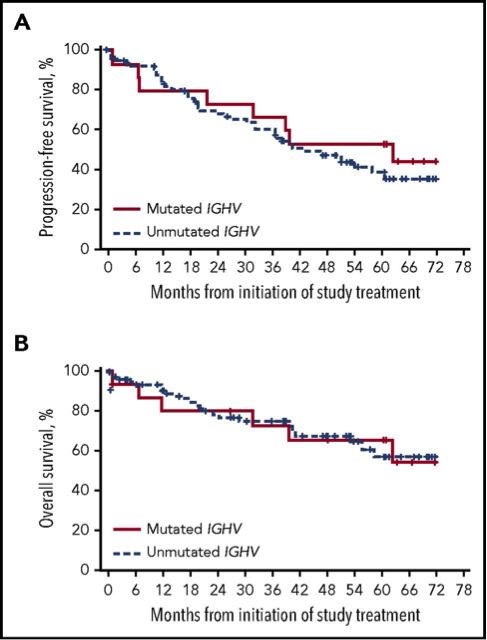
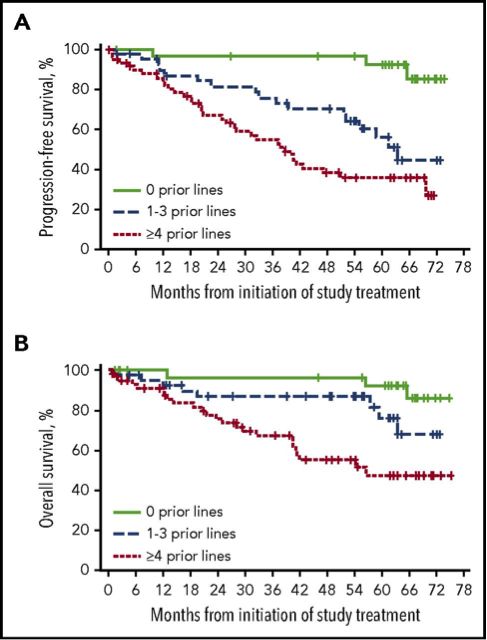
伊布替尼(ibrutinib)是一种布鲁顿酪氨酸激酶(BTK)抑制剂,已被批准用于CLL/SLL的单药治疗。伊布替尼治疗CLL/SLL有效率高、缓解时间长、毒副反应小。3年随访结果显示,其总体反应率为89% ,完全缓解率为11%。O’Brien等继续随访了伊布替尼单药治疗单药治疗CLL/SLL患者,重点观察了高危患者疗效、疗效影响因素、疗效质量及毒副作用,其研究结果近期发表在Blood上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#随访结果#
20
#单药治疗#
22
#淋巴细胞白血病#
25
#结果公布#
32
#5年随访#
53
不错
0
xuex
0
学习
61
学习了
59
#伊布替尼#
25