Hepatology:王红阳院士发现肝癌患者中红细胞增多症的分子机制
2016-12-04 MedSci MedSci原创
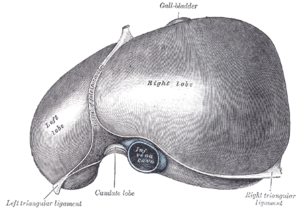
近日国际著名肝脏疾病杂志Hepatology在线发表了第二军医大学附属东方肝胆外科医院王红阳院士研究成果,癌细胞来源的促红细胞生成素在肝细胞癌的进展中发挥一定的作用,并且EPO/EPOR可被视为具有红细胞增多症的肝癌患者的一个治疗靶标。红细胞增多症(Erythrocytosis)与许多类型的肿瘤相关,包括肾细胞癌、脑膜瘤以及肝细胞癌(HCC)。红细胞增多症是HCC中最常见的一种副肿瘤性综合征,存在
近日国际著名肝脏疾病杂志Hepatology在线发表了第二军医大学附属东方肝胆外科医院王红阳院士研究成果,癌细胞来源的促红细胞生成素在肝细胞癌的进展中发挥一定的作用,并且EPO/EPOR可被视为具有红细胞增多症的肝癌患者的一个治疗靶标。
EPO是一种多效性细胞因子,调节着红细胞生成、血管生成、细胞保护和增殖。在成人当中,它主要是由肾脏的肾小管间质细胞产生的。然而,在胎儿发育阶段,肝脏是EPO的主要来源。EPO通过结合EPO受体(EPOR)而发挥作用,EPOR主要表达于红系祖细胞的表面。当缺乏EPO时,EPOR作为二聚体出现,并且与Janus激酶-2(JAK-2)酪氨酸激酶分子相关。在EPO结合后,EPOR的构象发生改变并激活JAK2相关信号转导级联反应,从而导致这些细胞的增殖、存活和分化。
EPOR在非造血细胞起源的肿瘤细胞系中表达,包括HCC、乳腺癌和宫颈癌,这是很值得关注的,因为合成的EPO经常被用来治疗癌性贫血,并能对肿瘤细胞产生不可逆转的增殖和/或存活效应。越来越多的临床前证据表明,内源性EPO可以促进肿瘤细胞增殖、干细胞的自我更新以及治疗的耐药性。同样,一些临床试验已经表明,在治疗过程中施用红细胞生成刺激剂,可减少无进展生存期(PFS)和总生存期(OS)。
为了调查某些肝癌患者中红细胞增多症发展的潜在机制,该研究小组对肿瘤和癌旁正常肝样本进行了全转录组和线粒体DNA(mtDNA)测序。他们发现,线粒体DNA突变导有助于缺氧诱导因子(HIF)的积累,由于三羧酸(TCA)循环代谢物的耗尽。持续增加HIF可诱导肝癌细胞强大的EPO表达和分泌,从而促进红细胞增多症和HCC的进展。为了阻断EPO/EPOR信号,研究人员使用一个EPOR胞外区Fc融合蛋白,并成功地在体外和体内抑制了肿瘤的生长。这些研究结果表明,癌细胞来源的促红细胞生成素在HCC的进展中发挥一定的作用,并且,EPO/EPOR应被视为具有红细胞增多症的肝癌患者的一个治疗靶标。
王红阳简介:
王红阳,中国工程院院士、发展中国家科学院(TWAS,原称第三世界科学院)院士,教育部长江"特聘教授" 。长期从事恶性肿瘤的基础与临床研究,对肿瘤发生发展的分子病理机制和细胞信号转导有重要建树。在Cancer Cell、J.E.M.、Gastroenterology(USA)、Hepatology、Cancer Res.、Nature 和Oncogene等有影响的主流期刊发表论文100多篇,总影响因子650;近五年申报发明专利28项,已获授权10项(国际专利1项)。以第一完成人获国家自然科学二等奖(2006)、何梁何利科技进步奖(2004)、上海医学科技一等奖(2003、2008)和上海市科技进步二等奖(2003)等7项,获2010年爱茉莉太平洋女科学家奖(韩国)、2009年度海内外最具影响力“中国妇女时代人物”、首届五洲女子科技奖、科学中国人(2007)年度人物奖、全国三八红旗手标兵、总后勤部“科技金星”、上海市“十大科技精英”和上海市“优秀学科带头人”等称号。担任国家自然科学基金委员会医学科学部主任、中国工程院医药卫生学部常委会委员、“癌基因及相关基因”国家重点实验室主任、全国生物化学与分子生物学学会副理事长、全军医学科技委员会副主任委员、全军生化专业委员会主任委员。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肝癌患者#
21
#王红阳#
30
EPO通过结合EPO受体(EPOR)而发挥作用,EPOR主要表达于红系祖细胞的表面。当缺乏EPO时,EPOR作为二聚体出现,并且与Janus激酶-2(JAK-2)酪氨酸激酶分子相关。在EPO结合后,EPOR的构象发生改变并激活JAK2相关信号转导级联反应,从而导致这些细胞的增殖、存活和分化。
44
中国人是有能力的。
51
#红细胞#
31
#EPA#
20
#红细胞增多症#
28
攻克癌症又向前迈进了一步
50
学习了,很好
48
继续关注
50