Hypertension:收缩压控制良好降高血压患者新发房颤风险
2015-07-02 小田 译 医学论坛网
既往研究已明确了高血压和心房颤动(以下简称房颤)的相关性;的确,即使是正常收缩压(SBP)高值水平也是房颤发生的长期预测因素。这些研究结果提示,采取更为积极的血压控制可能减少新发房颤风险。但实现较低水平的SBP是否与房颤发生率较低有关尚不清楚。因此,欧洲学者们对上述问题进行了研究。 研究纳入了8831例心电图证明左心室肥大但无房颤病史的高血压患者,
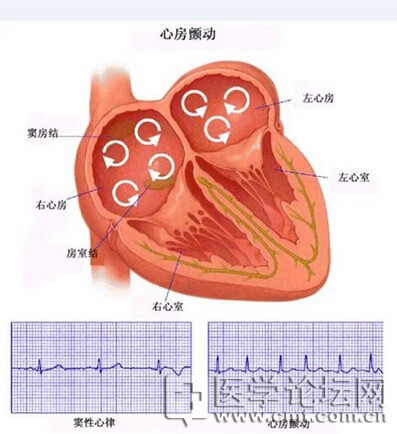
既往研究已明确了高血压和心房颤动(以下简称房颤)的相关性;的确,即使是正常收缩压(SBP)高值水平也是房颤发生的长期预测因素。这些研究结果提示,采取更为积极的血压控制可能减少新发房颤风险。但实现较低水平的SBP是否与房颤发生率较低有关尚不清楚。因此,欧洲学者们对上述问题进行了研究。
研究纳入了8831例心电图证明左心室肥大但无房颤病史的高血压患者,患者基线心电图显示为窦性心律,随机分为基于氯沙坦或阿替洛尔的治疗组,对其新发房颤风险进行评估。对SBP ≤130 mm Hg、SBP 131~141 mm Hg和≥142 mm Hg的患者进行比较。
结果显示,在随访的4.6±1.1年中,701例患者被诊断为新发房颤(7.9%)。在多变量Cox分析中,与治疗期间SBP ≥142 mm Hg相比,SBP ≤130 mm Hg、SBP 131~141 mm Hg作为时间变量分别与40%和24%的新发房颤风险较低有关。
该研究表明,实现SBP ≤130 mm Hg与心电图证实左心室肥厚高血压患者的新发房颤风险较低有关。需确定无房颤高血压患者SBP目标值的进一步研究可以减少高危人群新发房颤的负担。
相关研究论文6月8日在线发表于《高血压》(Hypertesion)杂志。

原始出处:
Okin PM1, Hille DA2, Larstorp AC2, Wachtell K2, Kjeldsen SE2, Dahlöf B2, Devereux RB2.Effect of Lower On-Treatment Systolic Blood Pressure on the Risk of Atrial Fibrillation in Hypertensive Patients.Hypertension.June 8, 2015. pii: HYPERTENSIONAHA.115.05728.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TENS#
21
#PE#
30
#收缩压#
32
进一步学习
73
看看
109
#高血压患者#
32
#新发房颤#
26
#Hypertension#
20
#房颤风险#
32
不错的
105