JBJS:脊髓麻醉与全麻实施初次全膝关节置换的短期并发症差异
2013-04-30 JBJS dxy
以往多项研究表明 [1-7],相比全麻,脊髓麻醉实施骨关节手术的术后深静脉血栓形成发生率更低,手术时间更短,手术失血量更少。最近,美国爱荷华大学医院及临床研究中心的Andrew J. Pugely, MD等实施了一项临床观察研究,对全膝关节置换患者应用全麻和脊髓麻醉的围手术期(30天内)并发症发生率及死亡率进行对比评价,他们的研究结果发表在最新一期的JBJS(Am)上,该研究的证据级别为治疗性研究
以往多项研究表明 [1-7],相比全麻,脊髓麻醉实施骨关节手术的术后深静脉血栓形成发生率更低,手术时间更短,手术失血量更少。最近,美国爱荷华大学医院及临床研究中心的Andrew J. Pugely, MD等实施了一项临床观察研究,对全膝关节置换患者应用全麻和脊髓麻醉的围手术期(30天内)并发症发生率及死亡率进行对比评价,他们的研究结果发表在最新一期的JBJS(Am)上,该研究的证据级别为治疗性研究III级。
通过美国大学外科医生全国外科手术质量改进项目(The American College of Surgeons National Surgical Quality Improvement Program, ACS NSQIP)数据库,检索2005年至2010年接受初次全膝关节置换术的病例资料,对术中采用全麻和脊髓麻醉患者的术后30天内并发症情况进行整理、评价。比较两种麻醉方式病例之间的一般特征、术后30天内并发症发生率以及死亡率,通过多变量Logistic回归分析,校正入选偏倚后确定术后30内并发症、死亡以及分层倾向评分的预测因素。
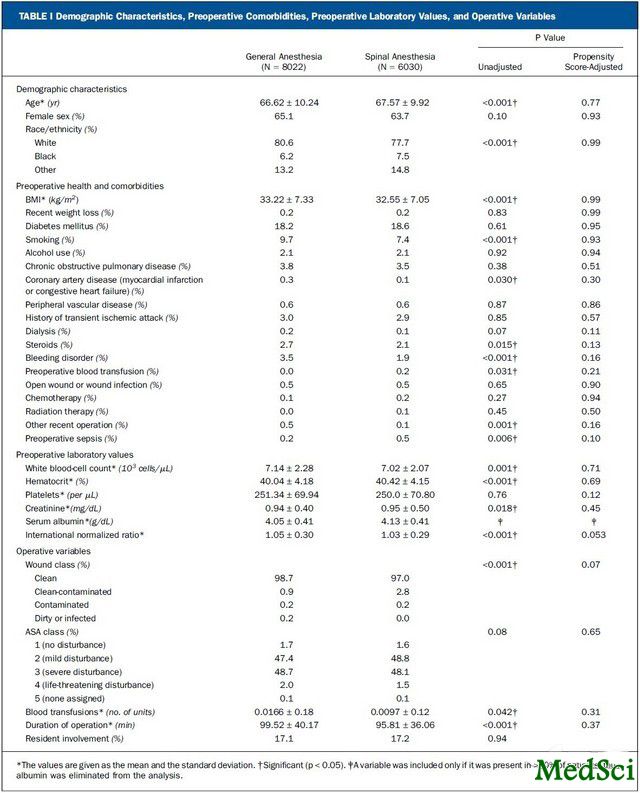
表 1.病例的人口统计学、术前合并症、术前实验室数据以及手术相关变量
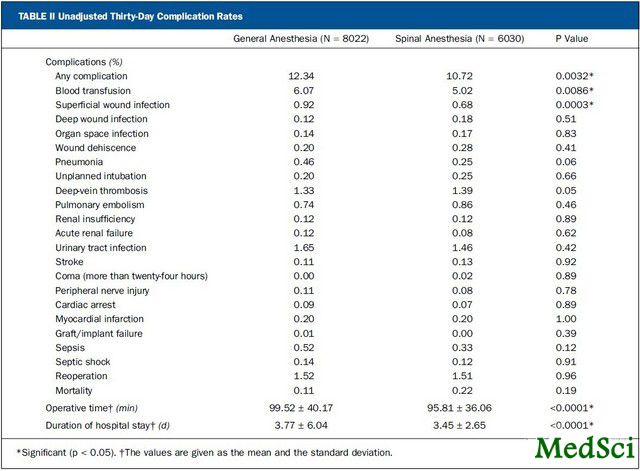
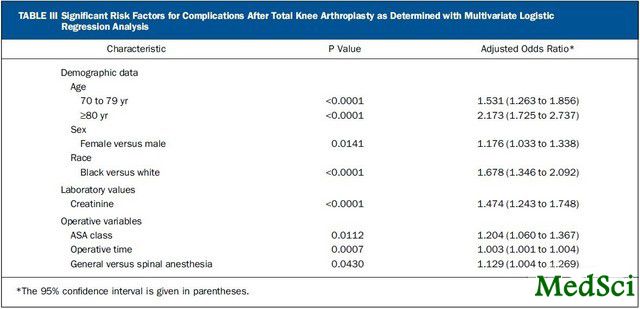
研究结果显示,共检索获得14,052例初次全膝关节置换患者的数据资料,其中6030 (42.9%)例采用脊髓麻醉,另外8022 (57.1%)例采用全麻实施手术。未对频数进行校正前,在切口浅表感染率(0.68% vs 0.92%; p = 0.0003)、输血率(5.02% vs 6.07%; p = 0.0086)以及总体并发症(10.72% vs 12.34%; p = 0.0032)发生率方面,以脊髓麻醉组患者显著更低。在手术时间(96 min vs 100 min; p < 0.0001)和住院时间(3.45天vs 3.77天; p < 0.0001)方面也以脊髓麻醉组患者更短。对潜在的混杂因素进行校正后,全麻施术患者的总体并发症发生概率显著更高(优势比,1.129;95%可信区间,1.004-1.269)。通过对术前合并症患病数量最多的患者进行分层评分五分之一匹配后证实,两组之间在术后短期并发症发生率方面差异显著(11.63% vs 15.28%; p = 0.0152)。另外,数据分析结果还表明,老龄、女性,黑色人种,肌酐升高,美国麻醉医师学会分级、手术时间以及麻醉方式选择是全膝关节置换术后短期并发症的独立风险因素。
表 3.经多变量Logistic回归分析确定的全膝关节置换术后并发症的风险因素
通过评价数据结果,作者认为,相比脊髓麻醉,全膝关节置换术中采用全麻会显著增加患者术后并发症的发生风险,通常这种差别较小,但术前存在多种合并症的患者差异是最大的,因此,对于存在多种合并症的患者,医生应考虑应用脊髓麻醉实施全膝关节置换手术。
与全膝关节置换相关的拓展阅读:
- AAOS 2013:全膝关节置换术(TKA)术后工作恢复率达99%
- JBJS:糖尿病患者全膝关节置换术后并无过高感染风险
- J Arthroplasty:后稳定型全膝关节置换术后前脱位 更多信息请点击:有关全膝关节置换更多资讯

Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty.
BACKGROUND
Spinal anesthesia has been associated with lower postoperative rates of deep-vein thrombosis, a shorter operative time, and less blood loss when compared with general anesthesia. The purpose of the present study was to identify differences in thirty-day perioperative morbidity and mortality between anesthesia choices among patients undergoing total knee arthroplasty.
METHODS
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database was searched to identify patients who underwent primary total knee arthroplasty between 2005 and 2010. Complications that occurred within thirty days after the procedure in patients who had been managed with either general or spinal anesthesia were identified. Patient characteristics, thirty-day complication rates, and mortality were compared. Multivariate logistic regression identified predictors of thirty-day morbidity, and stratified propensity scores were used to adjust for selection bias.
RESULTS
The database search identified 14,052 cases of primary total knee arthroplasty; 6030 (42.9%) were performed with the patient under spinal anesthesia and 8022 (57.1%) were performed with the patient under general anesthesia. The spinal anesthesia group had a lower unadjusted frequency of superficial wound infections (0.68% versus 0.92%; p = 0.0003), blood transfusions (5.02% versus 6.07%; p = 0.0086), and overall complications (10.72% versus 12.34%; p = 0.0032). The length of surgery (ninety-six versus 100 minutes; p < 0.0001) and the length of hospital stay (3.45 versus 3.77 days; p < 0.0001) were shorter in the spinal anesthesia group. After adjustment for potential confounders, the overall likelihood of complications was significantly higher in association with general anesthesia (odds ratio, 1.129; 95% confidence interval, 1.004 to 1.269). Patients with the highest number of preoperative comorbidities, as defined by propensity score-matched quintiles, demonstrated a significant difference between the groups with regard to the short-term complication rate (11.63% versus 15.28%; p = 0.0152). Age, female sex, black race, elevated creatinine, American Society of Anesthesiologists class, operative time, and anesthetic choice were all independent risk factors of short-term complication after total knee arthroplasty.
CONCLUSIONS
Patients undergoing total knee arthroplasty who were managed with general anesthesia had a small but significant increase in the risk of complications as compared with patients who were managed with spinal anesthesia; the difference was greatest for patients with multiple comorbidities. Surgeons who perform knee arthroplasty may consider spinal anesthesia for patients with comorbidities.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








很好的比较,学习了。
37
#脊髓麻醉#
40
#置换#
31
#并发#
30
#全麻#
37
#全膝关节置换#
35
#JBJS#
29