ACS Nano:可被人体吸收的新型心脏支架
2015-05-29 佚名 生物谷
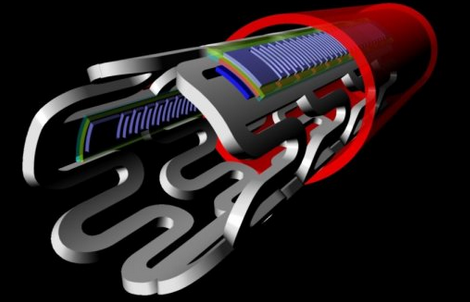
据统计,每年大约有50万美国人因斑块冠状动脉狭窄而接受支架支撑手术。但是手术并不是万无一失的,有时病人在手术后网状管道也会偶尔被阻塞。科学家们在《ACS Nano》杂志上发表的相关文章记录了一种新型多功能心脏支架,该支架可以使病人在治疗的整个过程中得到的风险最小。新型支架可以感觉到人体血液的流动和人体血液温度,而且能够对人体内存储和传输的信息进行分析,最后在完成它的使命后可被人体吸收。全世界医生为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










看看
131
#ACS#
25
#心脏支架#
37
高端
106
对于分叉病变可吸收支架应该有一定的优势
107
有待研究
128
。
98
个人感觉意义不大!
86