Stem Cells Int:用外泌体修补“破碎”的心脏
2017-12-11 土豆 “外泌体之家”微信号
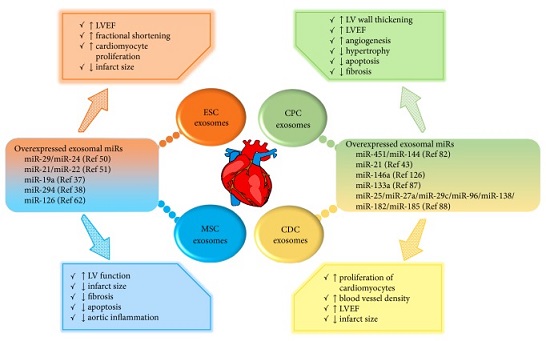
干细胞移植治疗是一种很有前景的修复损伤心脏组织并使其再生的辅助手段;然而,由于缺血心脏中移植细胞的存活不佳,一般仅能观察到心脏功能的适度改善。因此,对于可以帮助减轻心脏损伤的新疗法亟待出现。最近的研究已经证明干细胞释放的外泌体可以作为心脏修复的潜在的无细胞治疗剂。曾经一度被认为仅仅是一种细胞废物的外泌体或细胞外纳米粒子已被证明在包括短距离和长距离的细胞间通讯在内的生理功能中起着至关重要的作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#stem cells#
29
#CEL#
36
#stem cell#
30
#Cell#
30
#STEM#
21
#cells#
20